Communitization Initiatives in Bihar: Challenges Ahead
T he State of Bihar, with a
population density of 880
persons per sq. km. has recorded the
highest decadal growth during the
nineties (Census, 2001) with around
33% of its population below
poverty line. The major health and
demographic indicators of the State
like infant mortality rate, maternal
mortality ratio, total fertility rate, etc.
are much higher than at all India level,
which reflect poor health status in the
State. Amongst the major States, the
Human Development Index (HDI) in
Bihar has been the lowest for the last
three decades (UNDP, 2001). The
recent National Family Health Survey
(NFHS-III, 2005-06) indicates some
improvements in immunization
coverage, contraceptive use,
institutional deliveries and the
proportion of women, who have
awareness about HIV/AIDS.
However, malnutrition among
children and women has increased.
The prevalence of certain vector
borne diseases, communicable
diseases and water borne diseases is
also high in the State.
There are substantial gaps in health
sector infrastructure and essential
health requirements in terms of
manpower, equipment, drugs and
consumables in primary health care
institutions. There is a drastic decline
in public health facilities for treatment
of non-hospitalized ailments in both
rural and urban areas. There are also
substantial gaps in sub-centers,
primary health centers, and a very
large gap in community health
centers along with shortage of
manpower, drugs and equipments for
Primary Health Care and inadequate
training facilities. Other factors
affecting the health status include:
very high fertility rate; low level of
institutional deliveries; high level of
maternal deaths; very low coverage
of full immunization; low level of
female literacy; and poor status of
family planning programme.
With the upgradation of health
infrastructure such as recruitment of
doctors on contract, outsourcing
diagnostic facilities, availability of free
medicines, provision of ambulance
services and through a mechanism of
web-based monitoring, better health
outcomes are expected in the State.
In a span of about a year, manifold
increase in OPD attendance has been
reported at the CHC/Block/PHC
level. A significant increase has also
been noted in terms of number of
patients attending government health
facilities, except at health sub-centre
level. In spite of appointment of
doctors and specialists at a large scale,
there is a need to appoint 5% more
Medical Officers at the PHC level,
60% Surgeons, 70% Obstetrics /
Gynecologists, 76% Pediatrician and
46% Physicians in order to fulfill the
gaps of human resources at different
levels. There is also need to recruit
13% more ANMs and 33% more staff
nurses at different levels to make the
health centers fully functional (State
Health Society, Bihar, 2009).
The eleventh five year plan for the
State aimed to reduce IMR from
present 61 to 29 by the end of
Eleventh Plan. It is to be achieved
through emphasis on home based
newborn care, improving breast
feeding practices, integrated
management of neonatal and
childhood illnesses and increasing
immunization coverage. With the
efforts of the State, an increase in
immunization coverage has already
been observed. The goal of reducing
MMR from 371 per 100,000 live
births to123 by the end of the 11th
Plan is a formidable task. Yet, the
State would be making all efforts to
achieve that goal. With the
operationalization of Janani Evam Bal
Suraksha Yojana, the institutional
deliveries are increasing significantly.
Besides, efforts are being made to
improve antenatal care, provide
skilled attendance at delivery and
enhance facilities for emergency
obstetric care. The State is also trying
to reduce TFR from 4.0 to 3.0 by
the end of Eleventh Plan through
behavioral change communication to
bring about increase in the age at
marriage of girls, delaying first child
birth, greater male participation and
meeting the unmet need for family
planning through improved
infrastructure and organization of
family planning camps and other
service delivery measures.
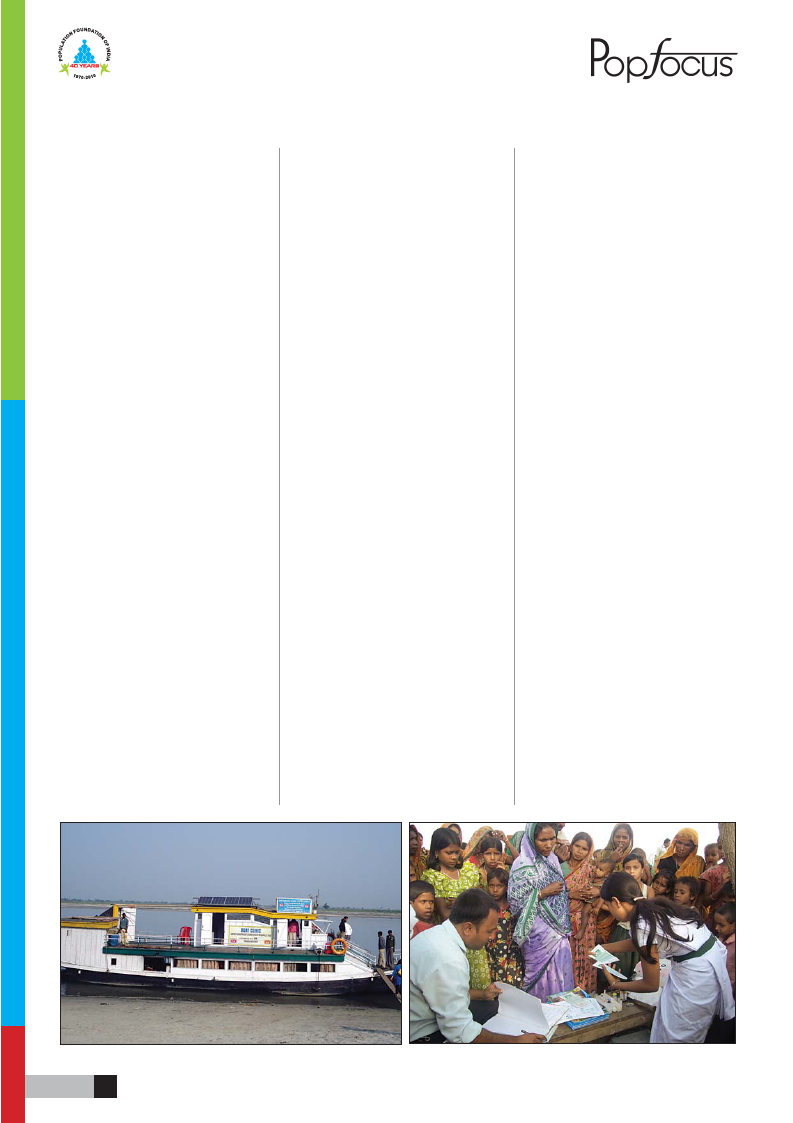
The National Rural Health Mission,
the flagship programme of the
Government of India has been a
facilitating factor and is expected to
improve the health system of the
State further. In Bihar, NRHM has
been launched to provide accessible,
affordable, accountable, effective and
reliable primary health care facilities,
especially to the poor and vulnerable
sections of the population. The aim
is to bridge the gap that exists in rural
health care services through the
creation of a cadre of Accredited
Social Health Activists (ASHAs),
improved hospital care and
decentralization of programmes at the
district level to improve intra and
inter-sectoral convergence and
effective utilization of resources.
Further, an overarching umbrella has
been provided to the existing
programmes of health and family
welfare including RCH-II, malaria,
blindness, iodine deficiency disorders,
Filariasis, Kala Azar, T.B., Leprosy
and integrated disease surveillance.
The State has made remarkable
progress over the last three years by
adopting and implementing different
strategies at different levels resulting
in significant decrease in MMR and
IMR. The MMR has come down to
312 from 372 against 254 of India
and IMR has decreased to 56 from
62 against 53 of all India but still there
is need to plan and implement the
programmes effectively as the TFR
has increased to 3.9 from 3.7 against
2.7 of all India level and coverage of
full ANC has come down to 3.9%
from 4.3%. The National Disease
Control Programme is also showing
significant result.
Though several efforts are being
made towards improving the health
service delivery at one level, no
effort had been made towards
“communitization”, one of the most
important components under NRHM
and strengthening the public health
system. Since the launch of
the NRHM, no Village Health &
Contd. on page 7
5