|
Infant Mortality Relation to Fertility FPF IDRC |
 |
1 Pages 1-10 |
▲back to top |
 |
1.1 Page 1 |
▲back to top |

 |
1.2 Page 2 |
▲back to top |
 |
1.3 Page 3 |
▲back to top |
 |
1.4 Page 4 |
▲back to top |
 |
1.5 Page 5 |
▲back to top |
 |
1.6 Page 6 |
▲back to top |
 |
1.7 Page 7 |
▲back to top |
 |
1.8 Page 8 |
▲back to top |
 |
1.9 Page 9 |
▲back to top |
 |
1.10 Page 10 |
▲back to top |
 |
2 Pages 11-20 |
▲back to top |
 |
2.1 Page 11 |
▲back to top |
 |
2.2 Page 12 |
▲back to top |
 |
2.3 Page 13 |
▲back to top |
 |
2.4 Page 14 |
▲back to top |
 |
2.5 Page 15 |
▲back to top |
 |
2.6 Page 16 |
▲back to top |
 |
2.7 Page 17 |
▲back to top |
 |
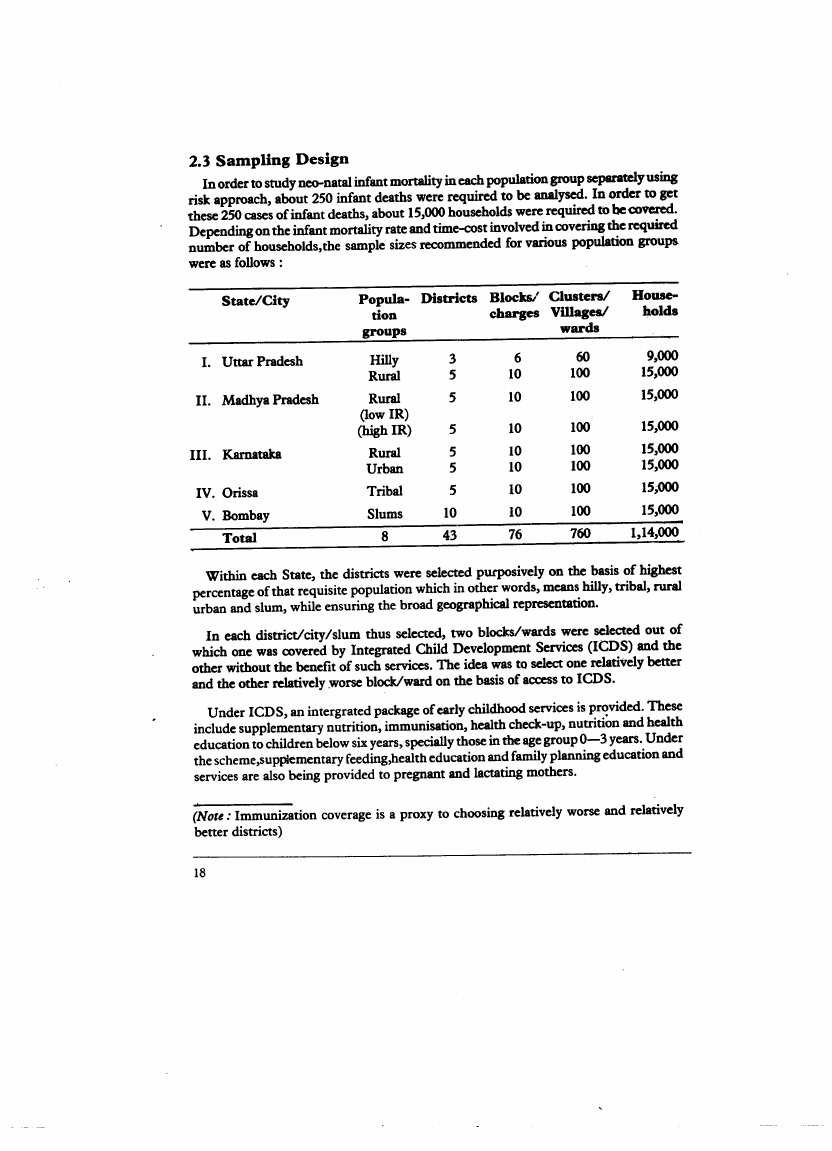
2.8 Page 18 |
▲back to top |
 |
2.9 Page 19 |
▲back to top |
 |
2.10 Page 20 |
▲back to top |
 |
3 Pages 21-30 |
▲back to top |
 |
3.1 Page 21 |
▲back to top |
 |
3.2 Page 22 |
▲back to top |
 |
3.3 Page 23 |
▲back to top |
 |
3.4 Page 24 |
▲back to top |
 |
3.5 Page 25 |
▲back to top |
 |
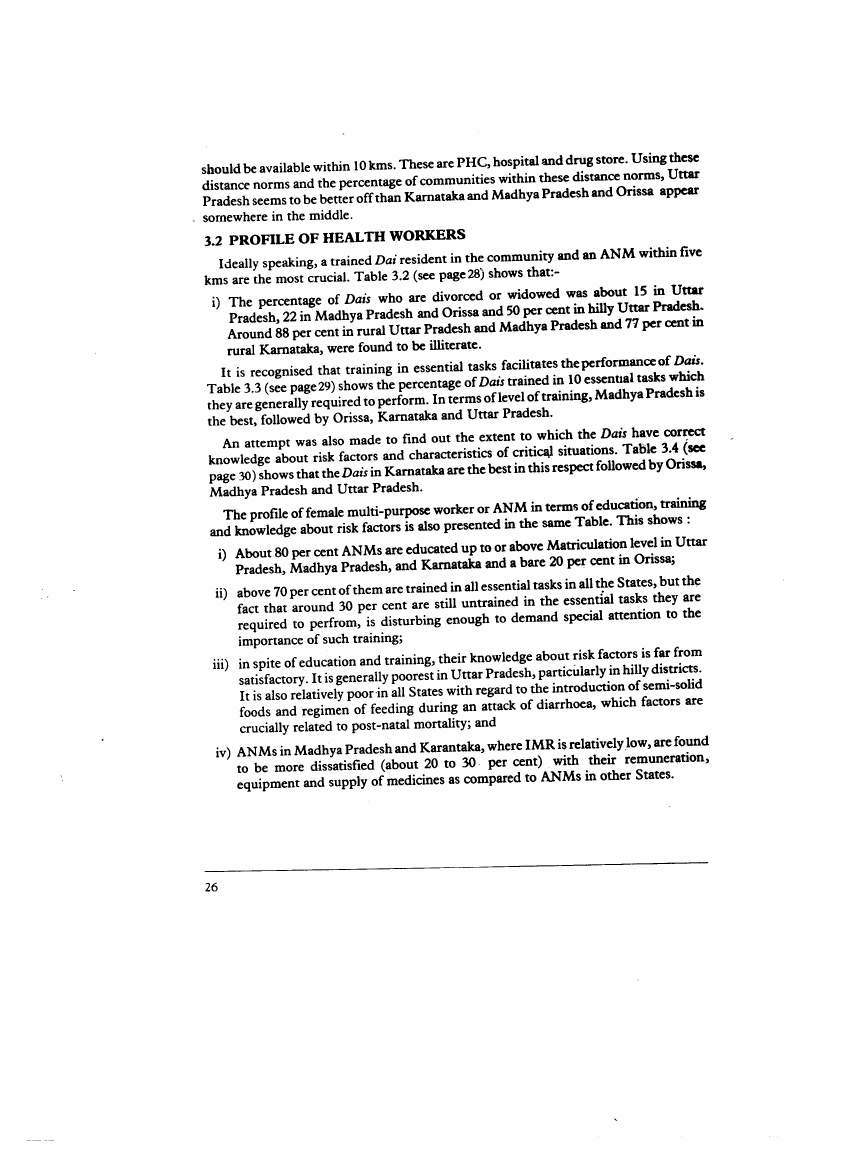
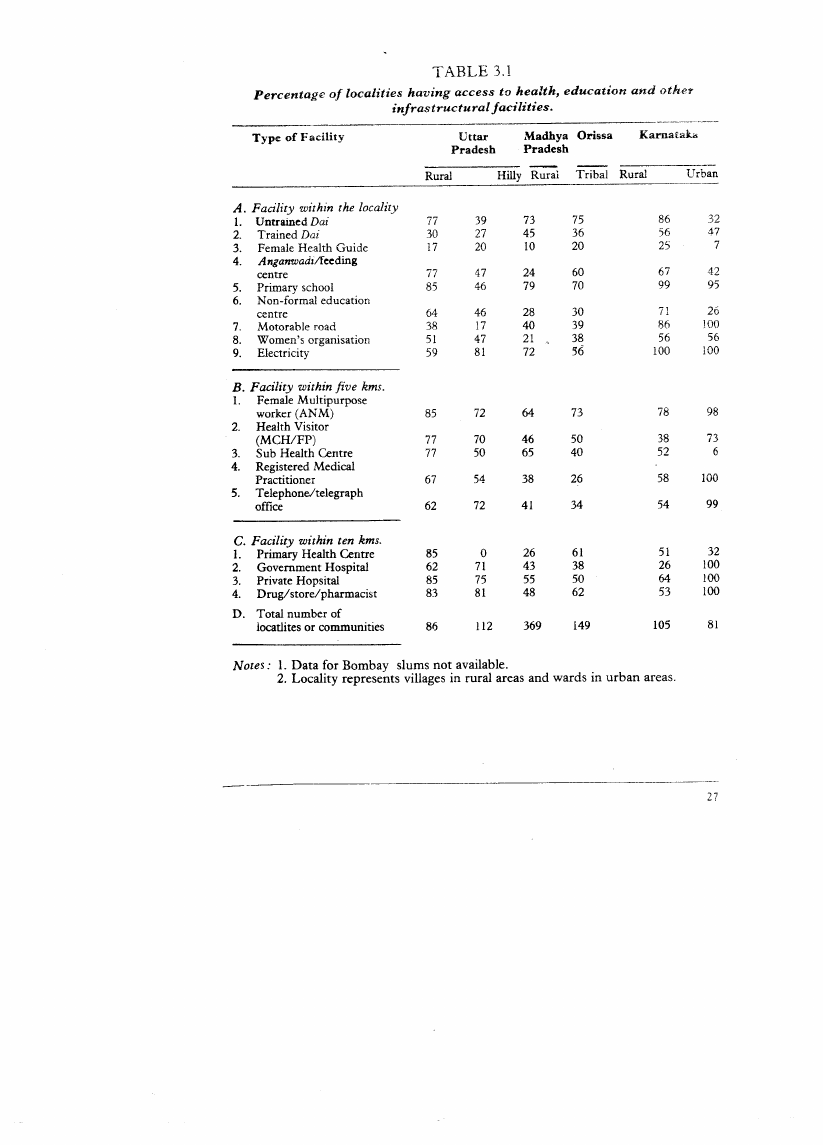
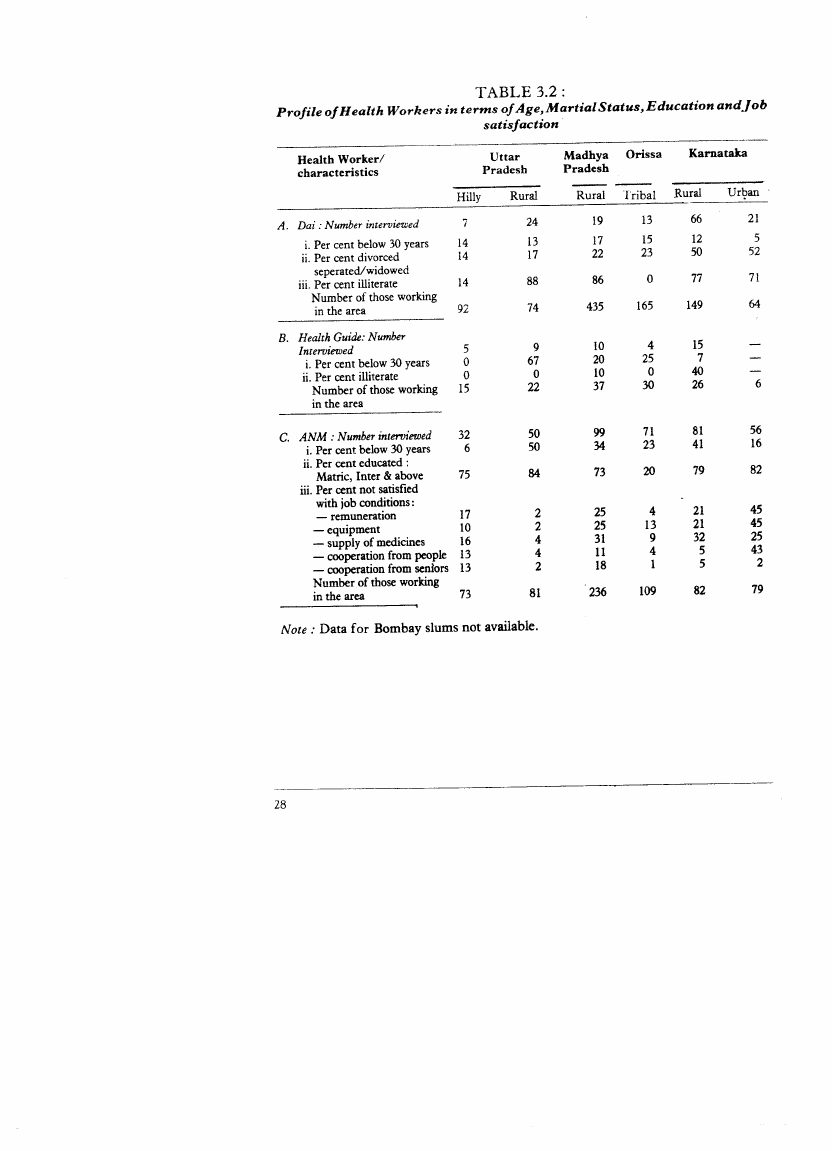
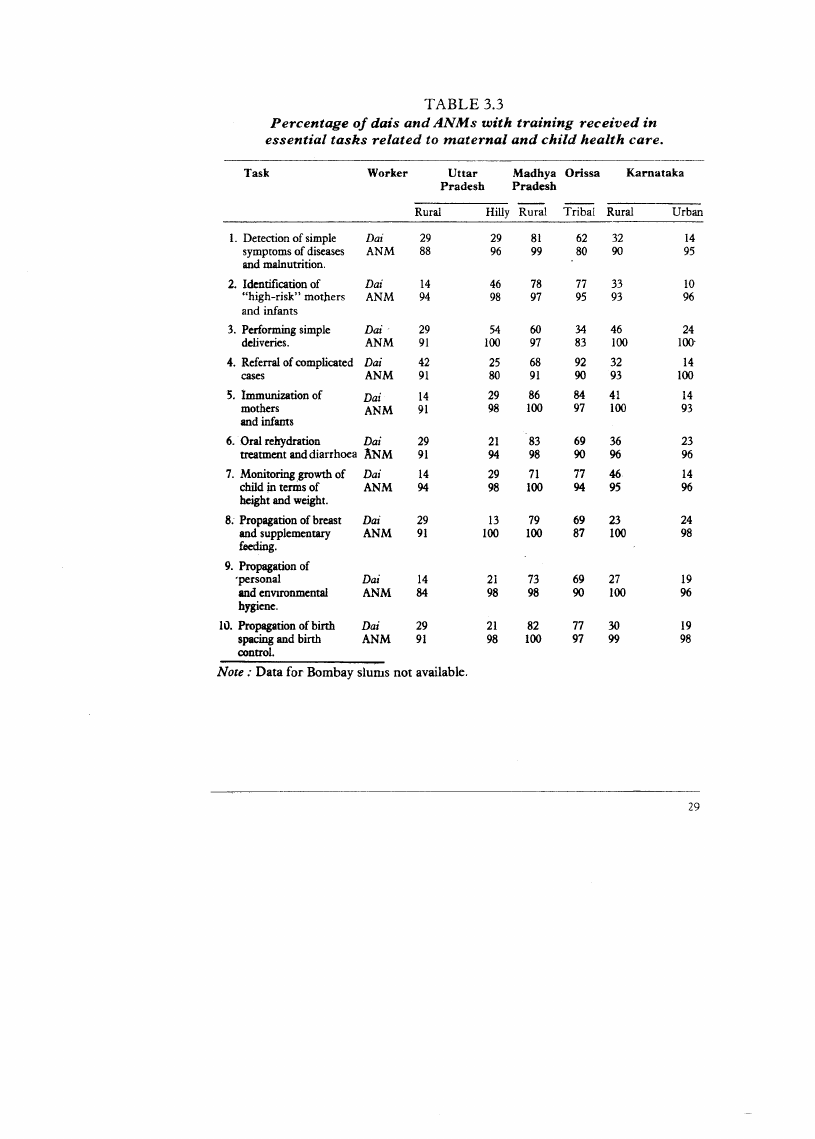
3.6 Page 26 |
▲back to top |
 |
3.7 Page 27 |
▲back to top |
 |
3.8 Page 28 |
▲back to top |
 |
3.9 Page 29 |
▲back to top |
 |
3.10 Page 30 |
▲back to top |
 |
4 Pages 31-40 |
▲back to top |
 |
4.1 Page 31 |
▲back to top |
 |
4.2 Page 32 |
▲back to top |
 |
4.3 Page 33 |
▲back to top |
 |
4.4 Page 34 |
▲back to top |
 |
4.5 Page 35 |
▲back to top |
 |
4.6 Page 36 |
▲back to top |
 |
4.7 Page 37 |
▲back to top |
 |
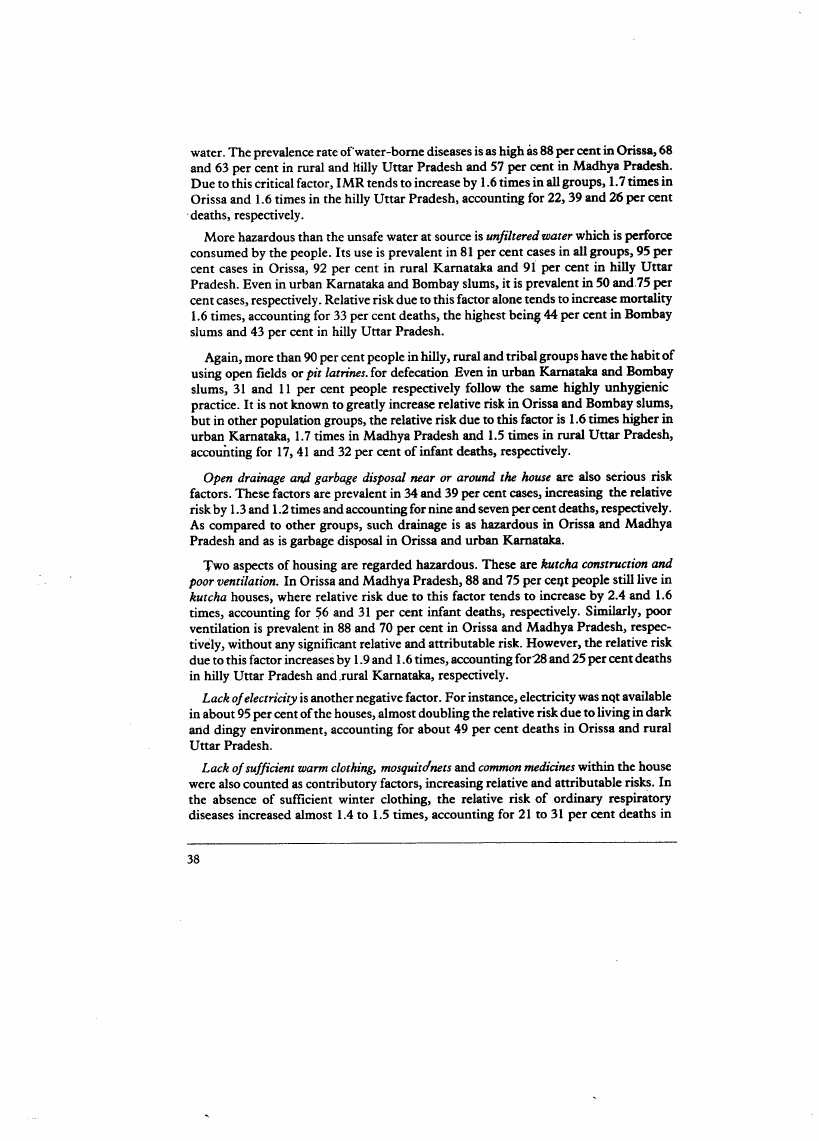
4.8 Page 38 |
▲back to top |
 |
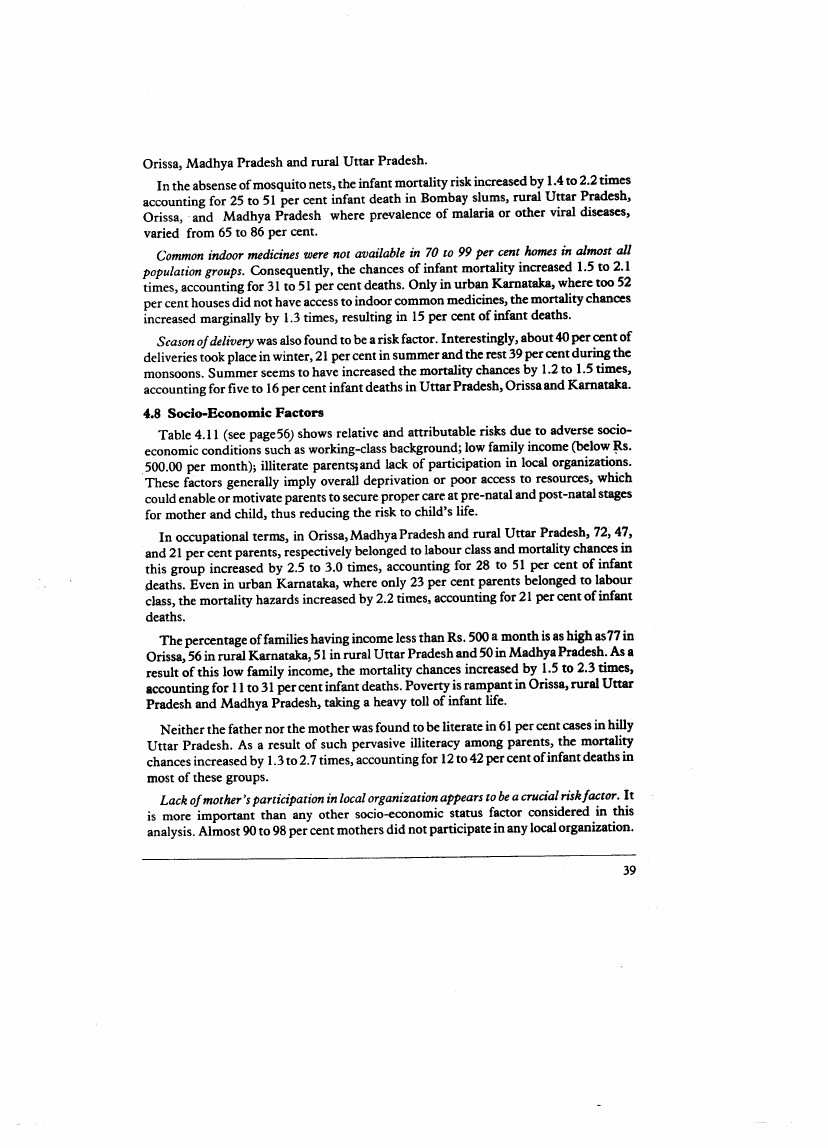
4.9 Page 39 |
▲back to top |
 |
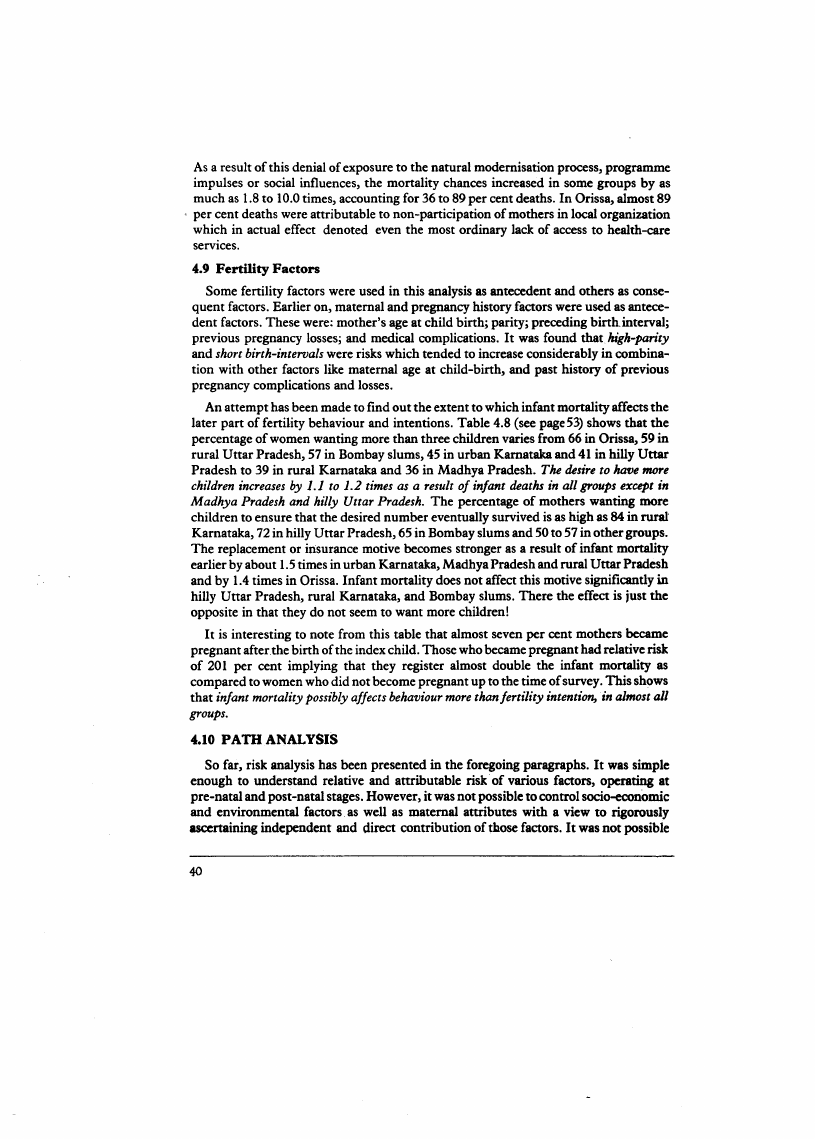
4.10 Page 40 |
▲back to top |
 |
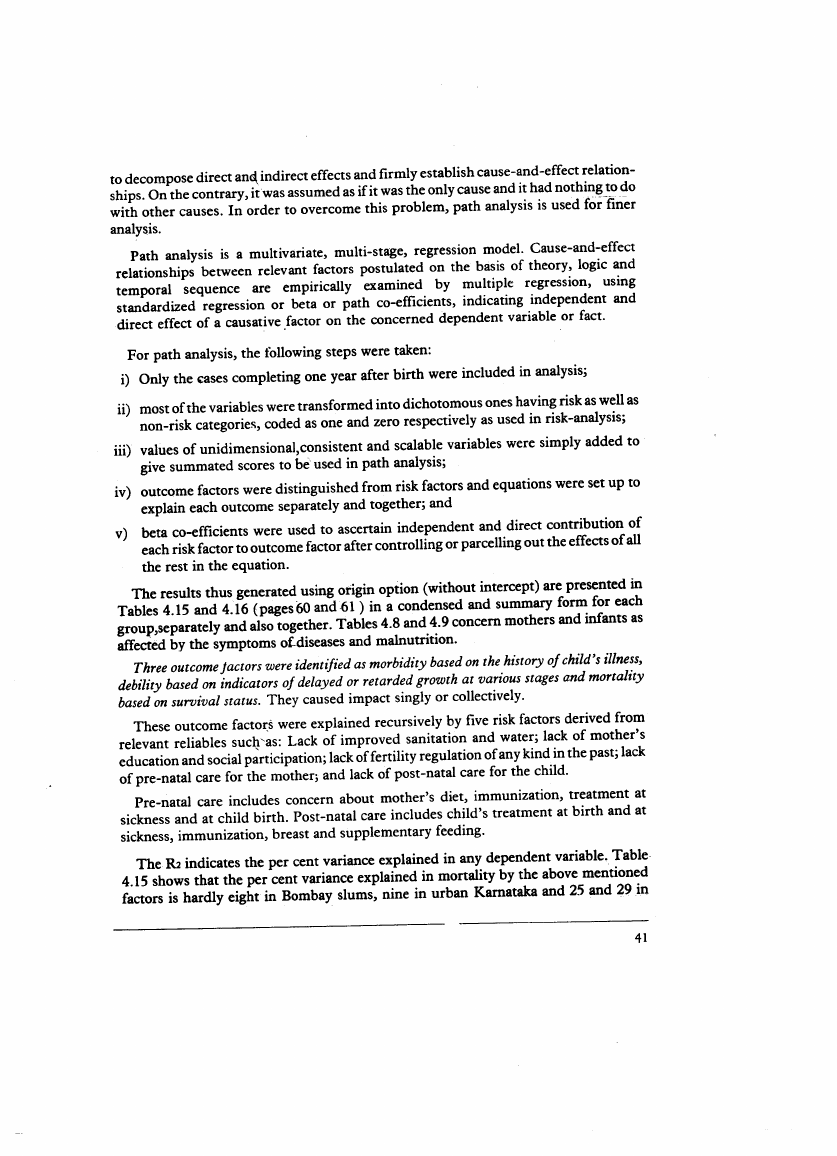
5 Pages 41-50 |
▲back to top |
 |
5.1 Page 41 |
▲back to top |
 |
5.2 Page 42 |
▲back to top |
 |
5.3 Page 43 |
▲back to top |
 |
5.4 Page 44 |
▲back to top |
 |
5.5 Page 45 |
▲back to top |
 |
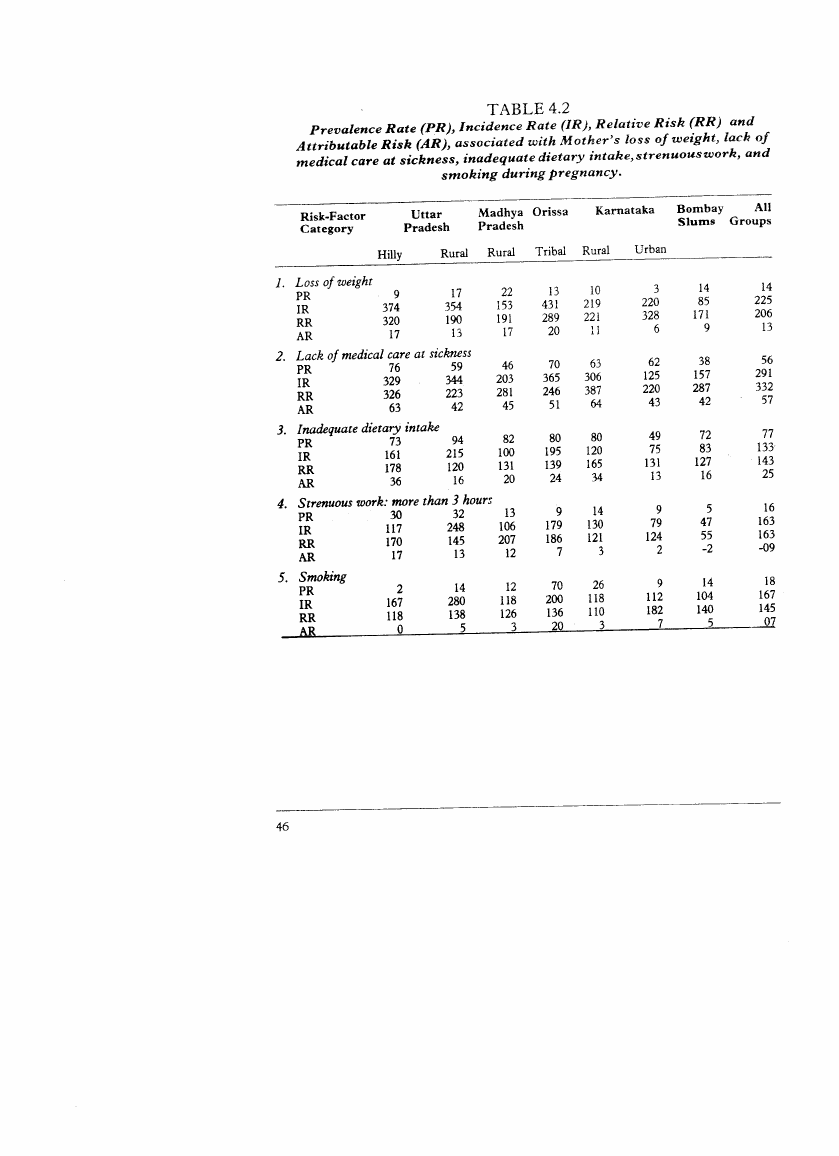
5.6 Page 46 |
▲back to top |
 |
5.7 Page 47 |
▲back to top |
 |
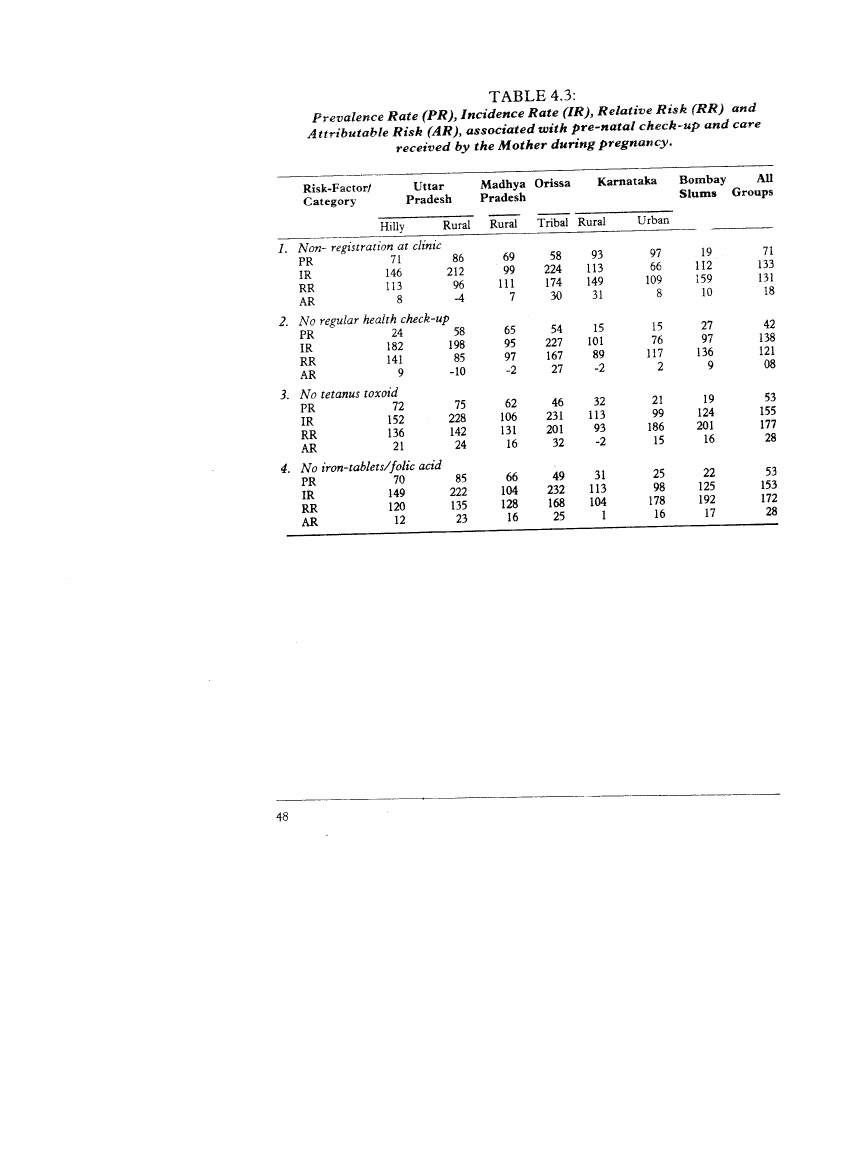
5.8 Page 48 |
▲back to top |
 |
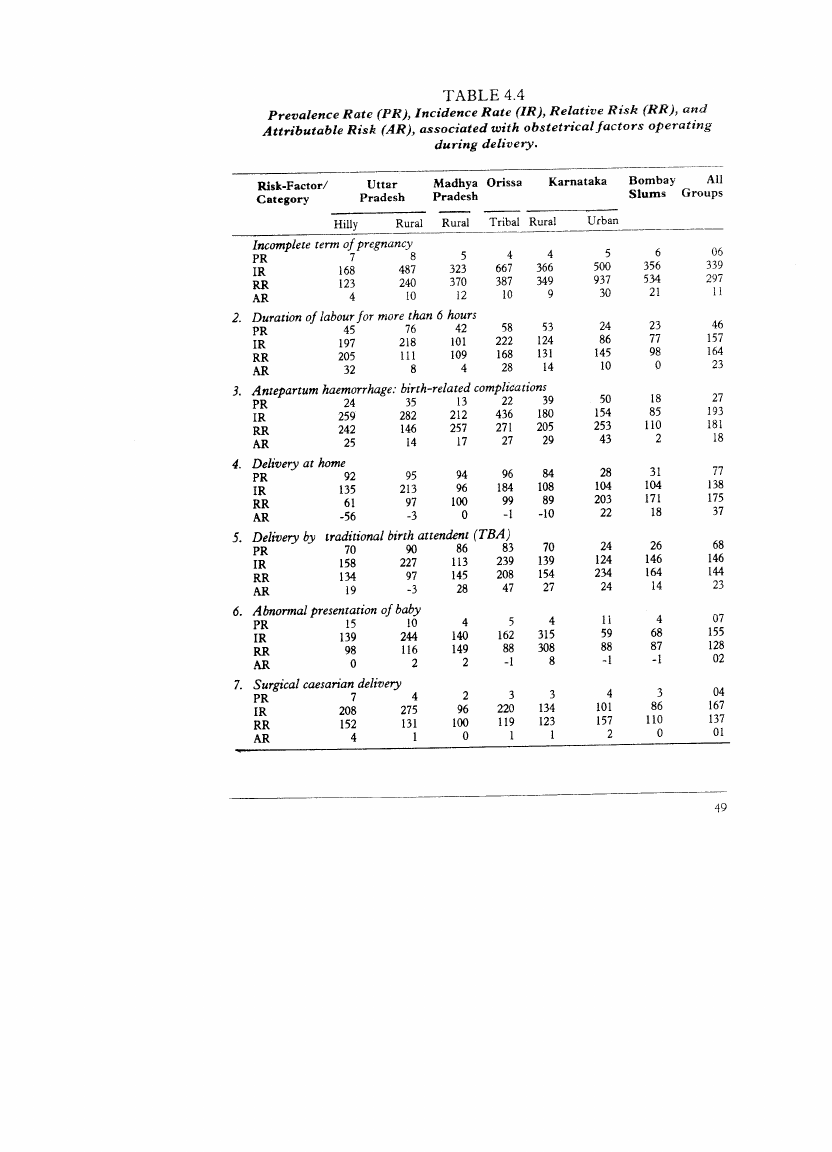
5.9 Page 49 |
▲back to top |
 |
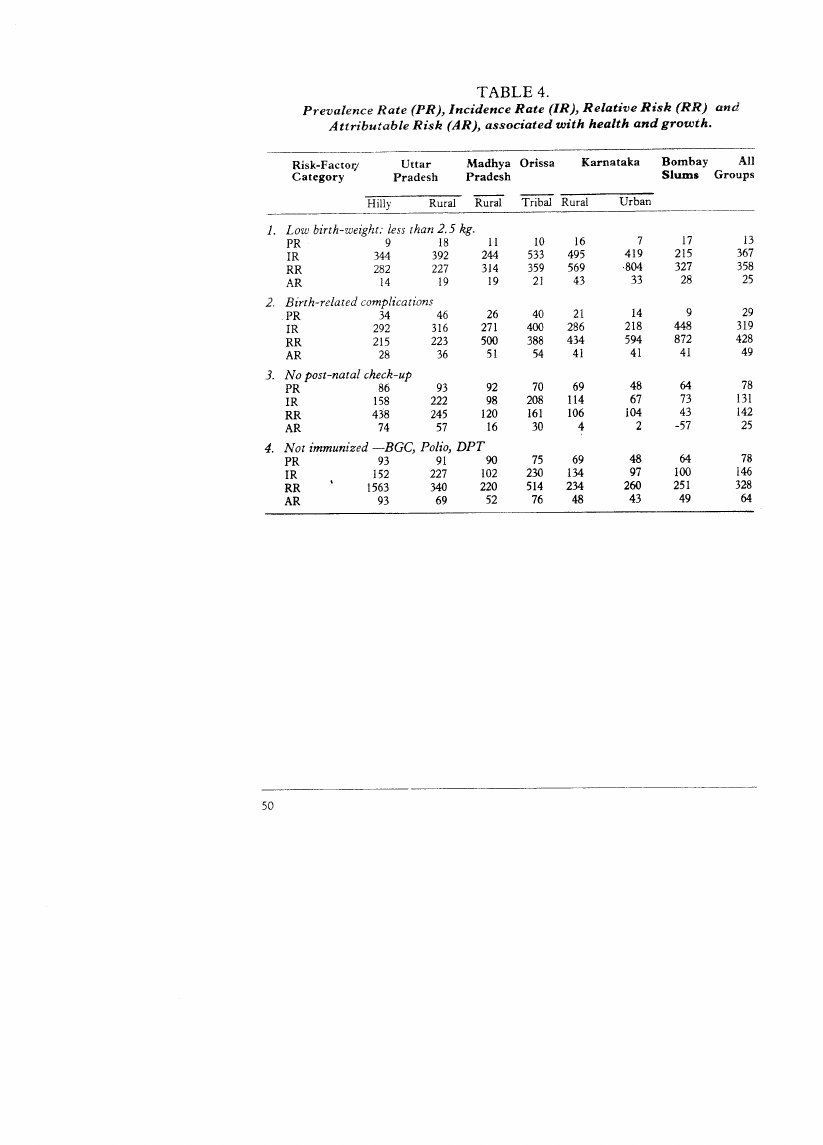
5.10 Page 50 |
▲back to top |
 |
6 Pages 51-60 |
▲back to top |
 |
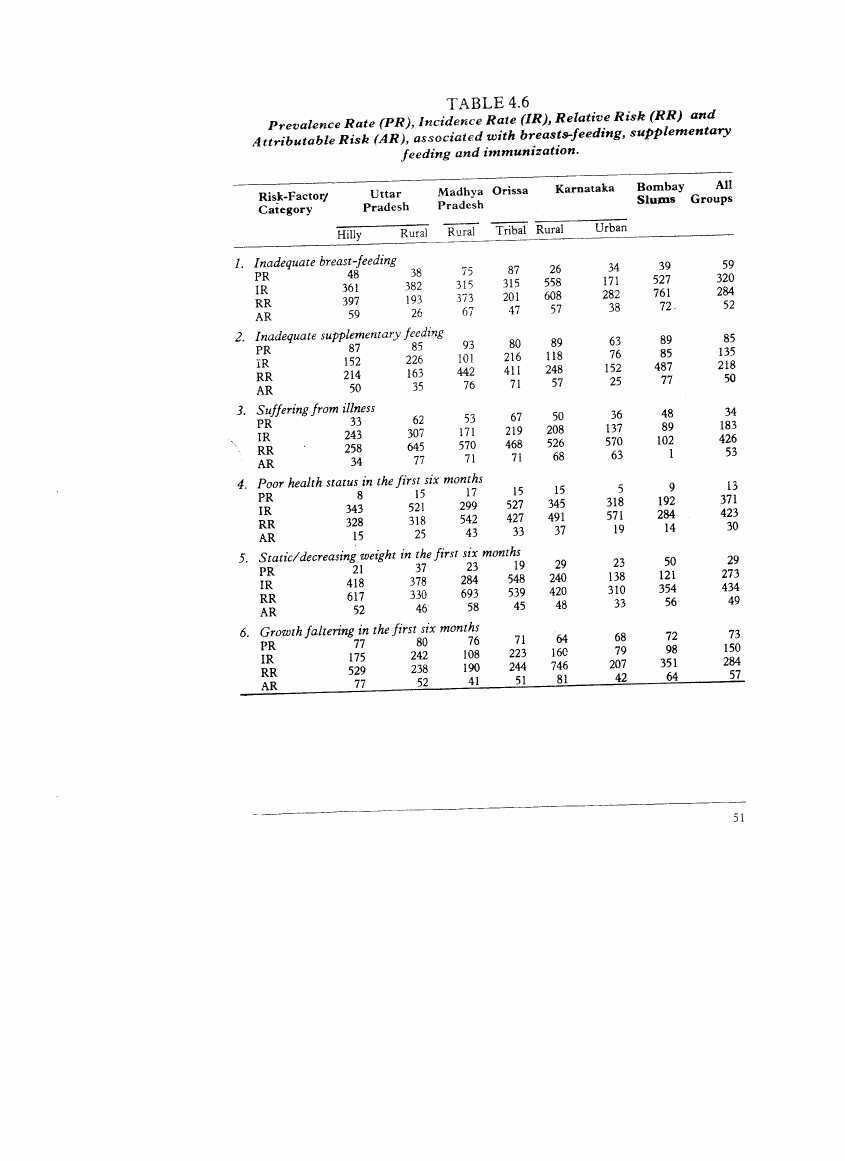
6.1 Page 51 |
▲back to top |
 |
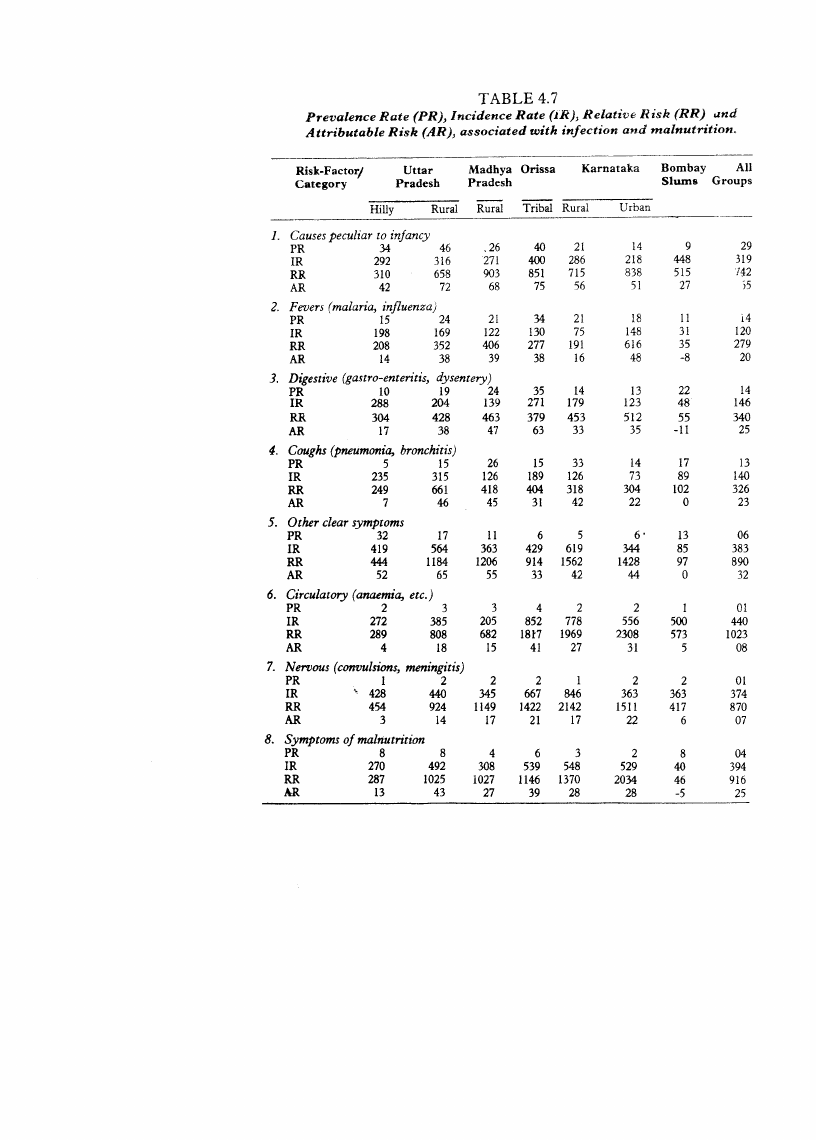
6.2 Page 52 |
▲back to top |
 |
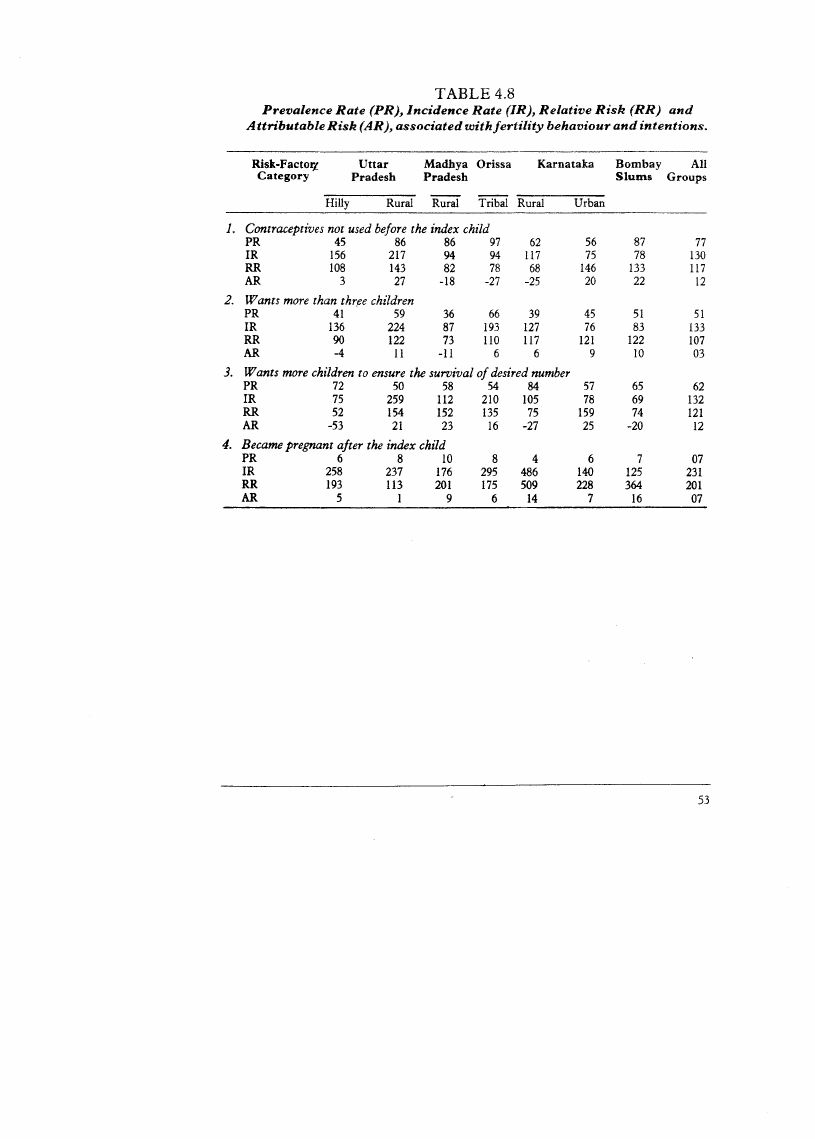
6.3 Page 53 |
▲back to top |
 |
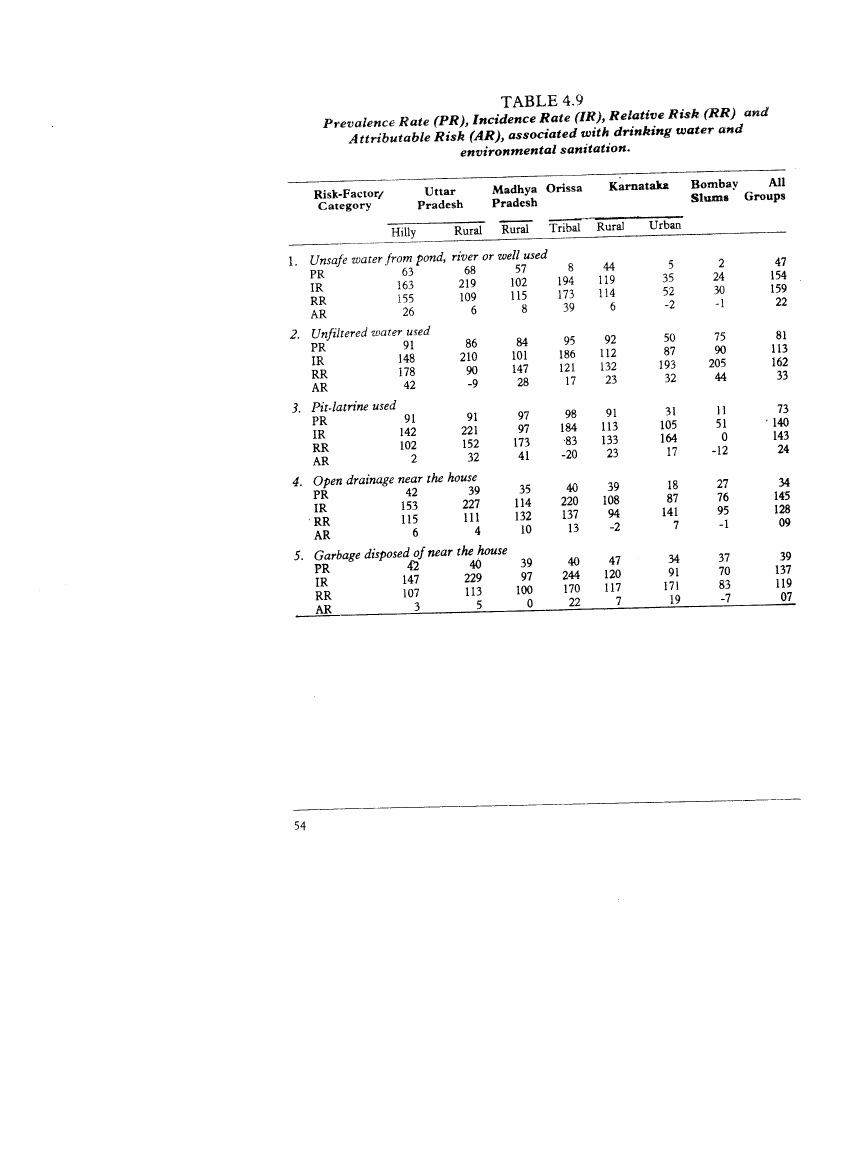
6.4 Page 54 |
▲back to top |

 |
6.5 Page 55 |
▲back to top |
 |
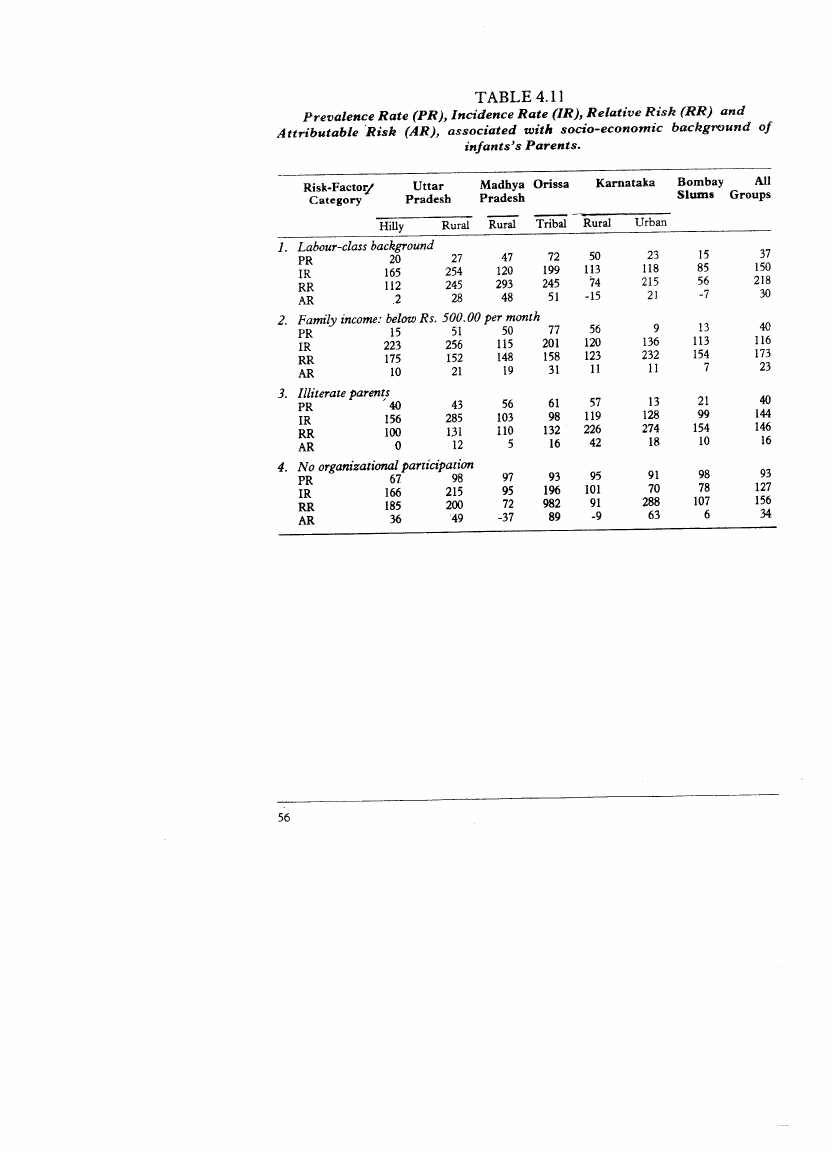
6.6 Page 56 |
▲back to top |
 |
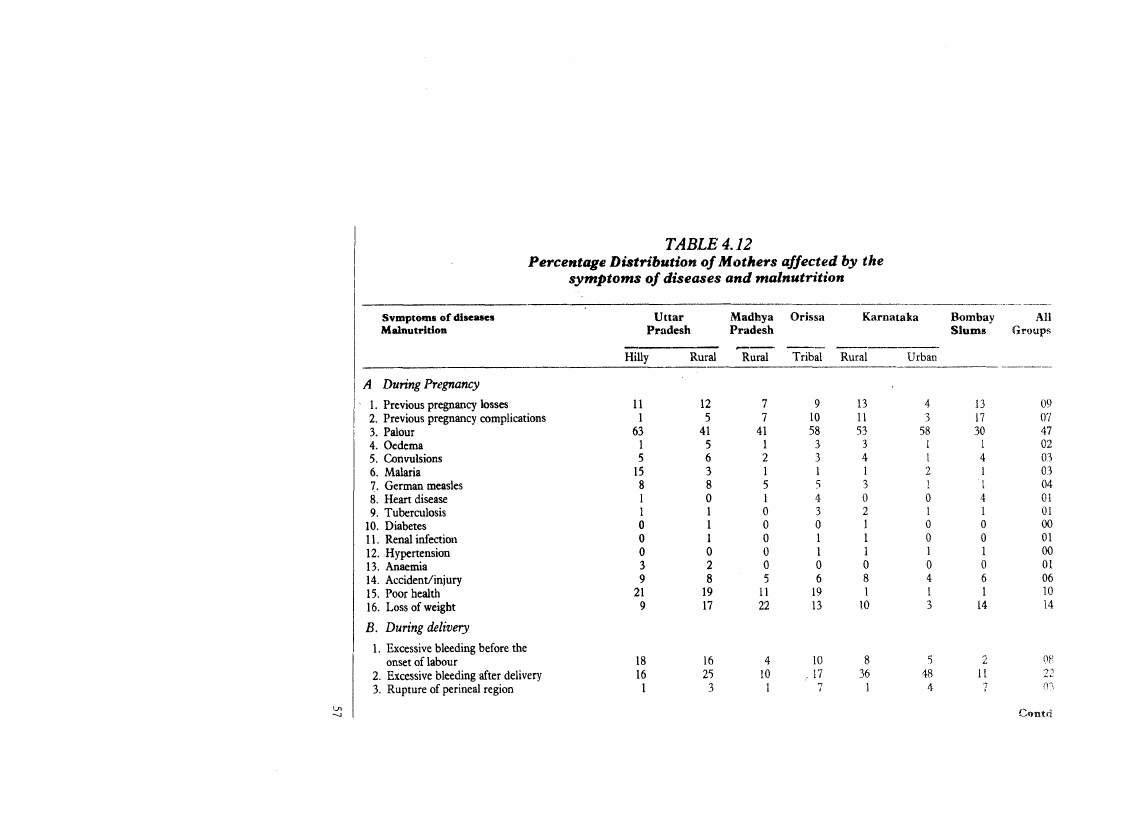
6.7 Page 57 |
▲back to top |
 |
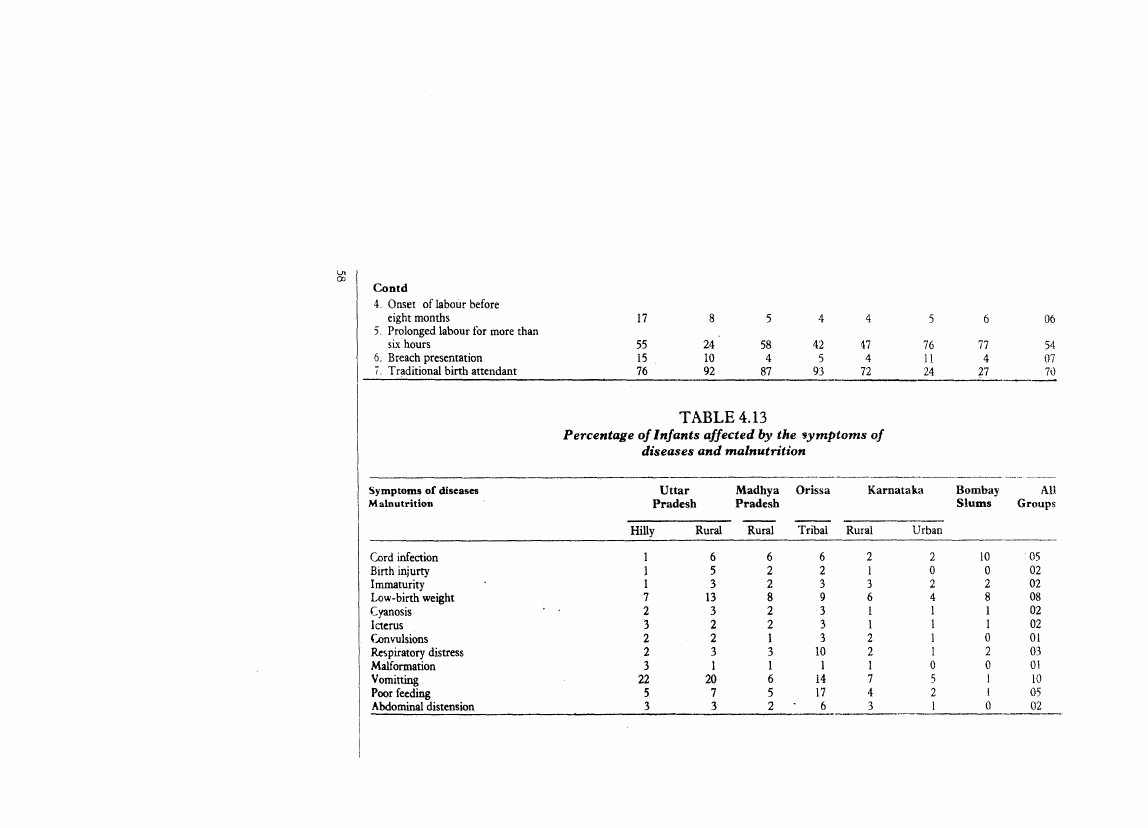
6.8 Page 58 |
▲back to top |
 |
6.9 Page 59 |
▲back to top |
 |
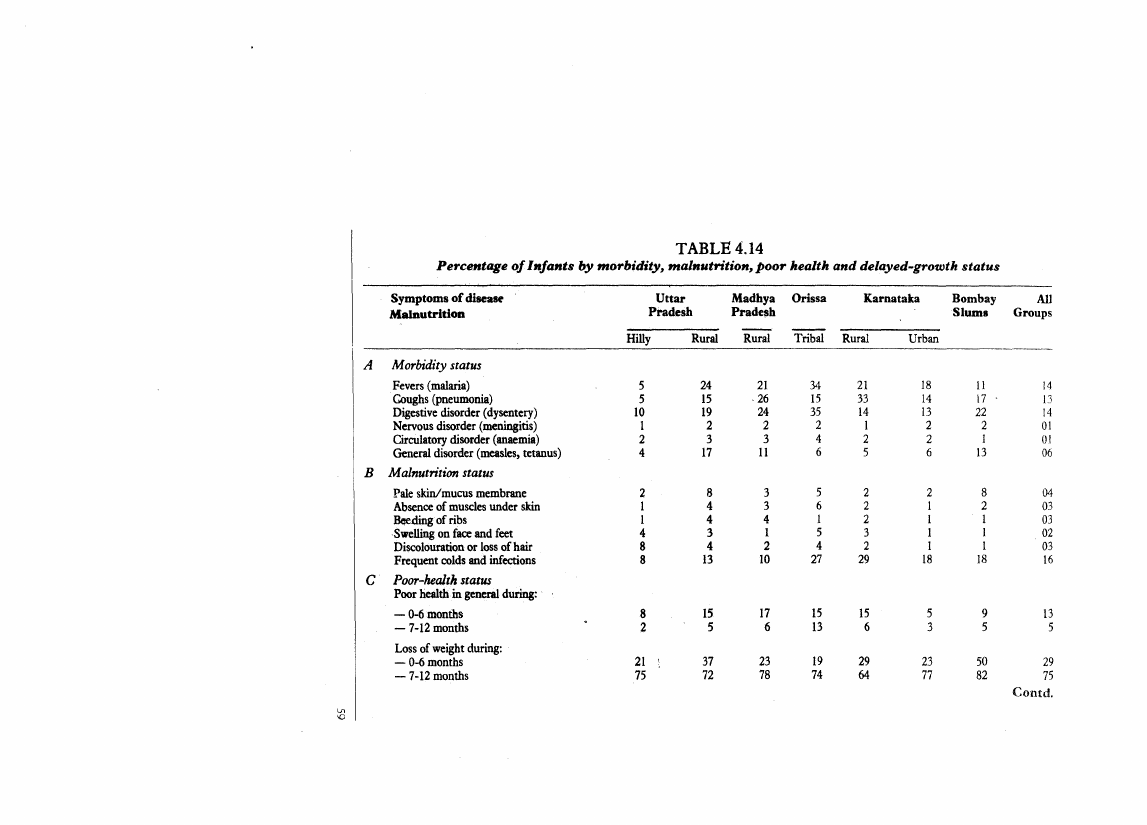
6.10 Page 60 |
▲back to top |
 |
7 Pages 61-70 |
▲back to top |
 |
7.1 Page 61 |
▲back to top |
 |
7.2 Page 62 |
▲back to top |

 |
7.3 Page 63 |
▲back to top |
 |
7.4 Page 64 |
▲back to top |
 |
7.5 Page 65 |
▲back to top |
 |
7.6 Page 66 |
▲back to top |
 |
7.7 Page 67 |
▲back to top |
 |
7.8 Page 68 |
▲back to top |
 |
7.9 Page 69 |
▲back to top |
 |
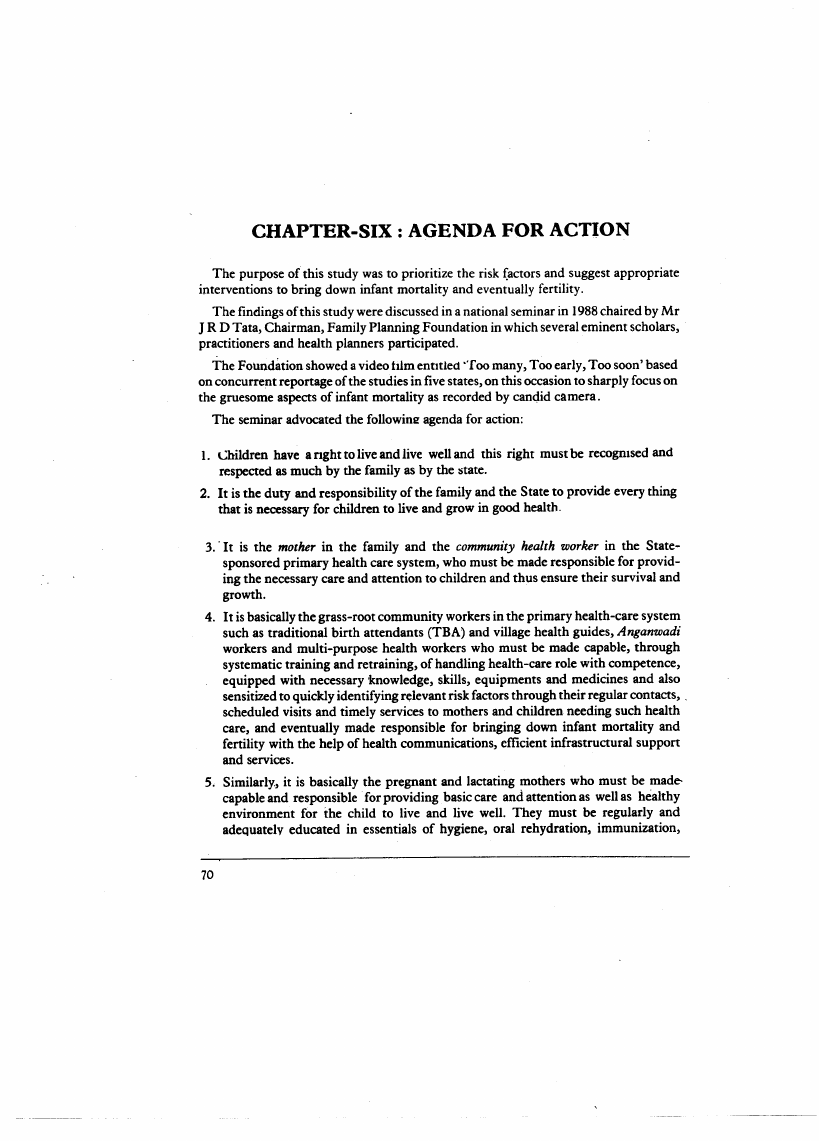
7.10 Page 70 |
▲back to top |
 |
8 Pages 71-80 |
▲back to top |
 |
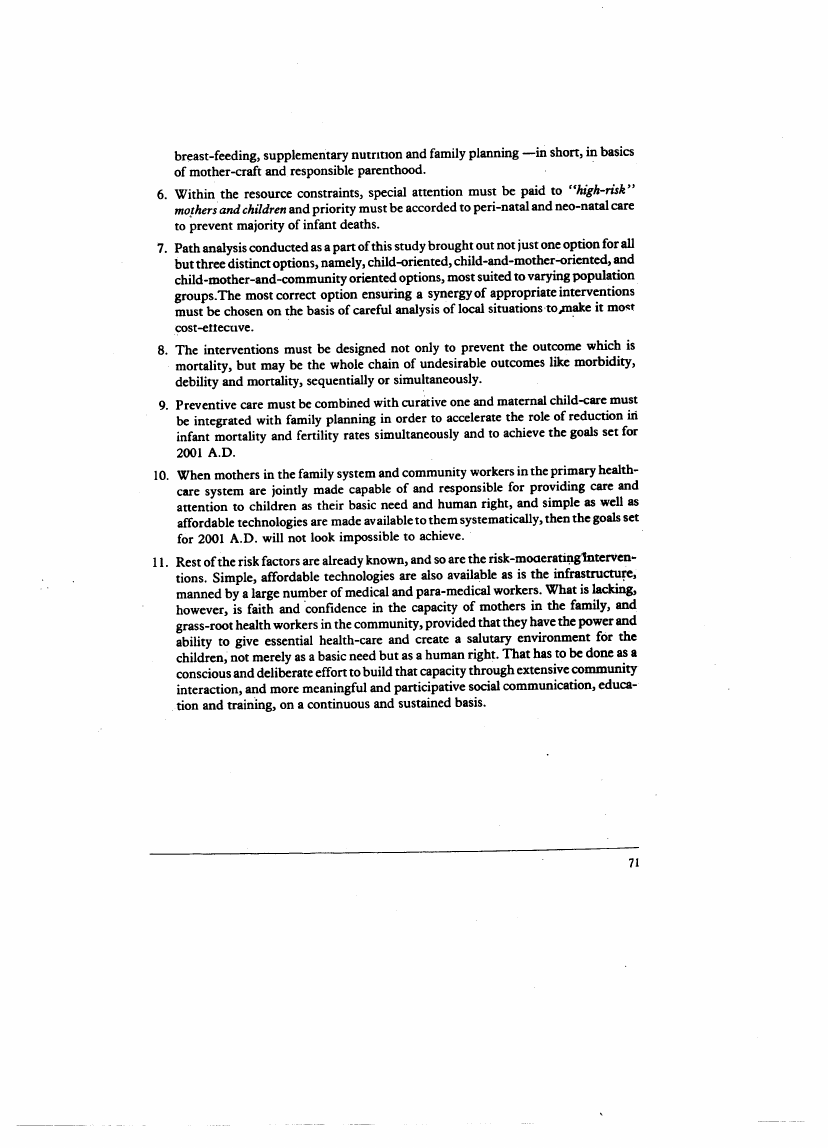
8.1 Page 71 |
▲back to top |
 |
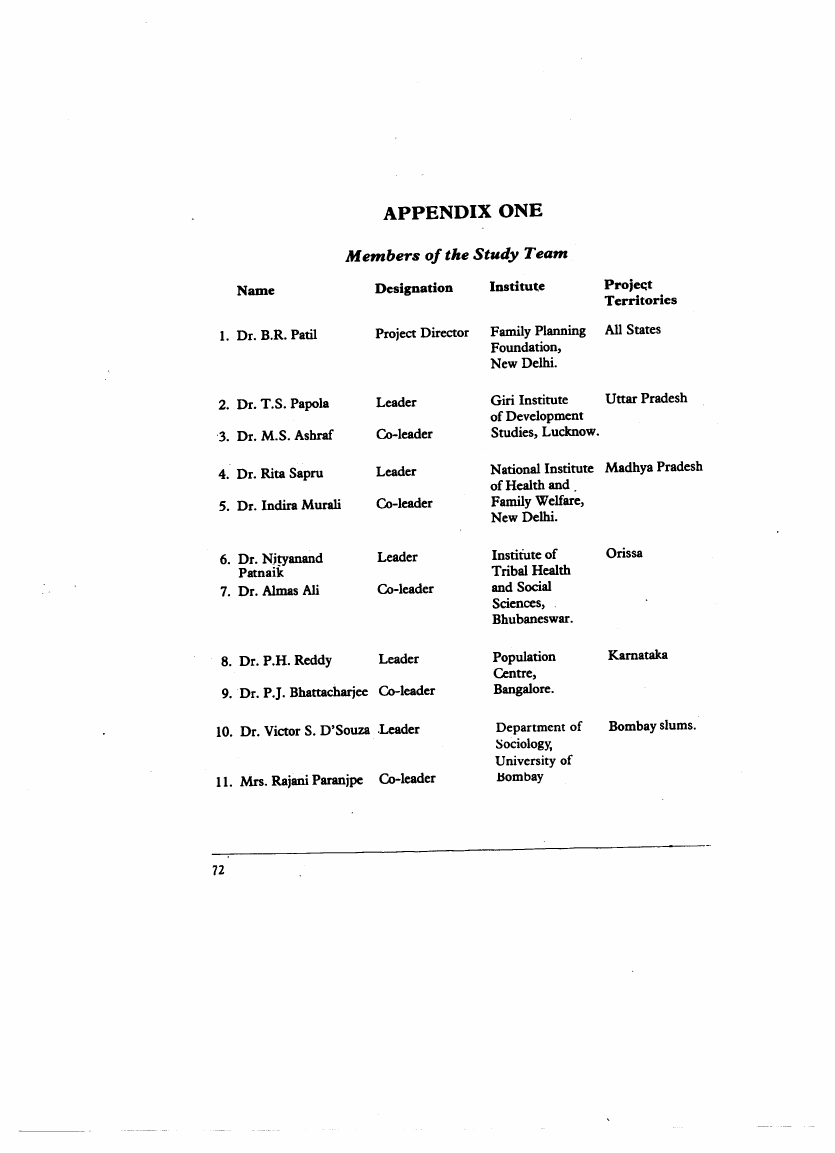
8.2 Page 72 |
▲back to top |
 |
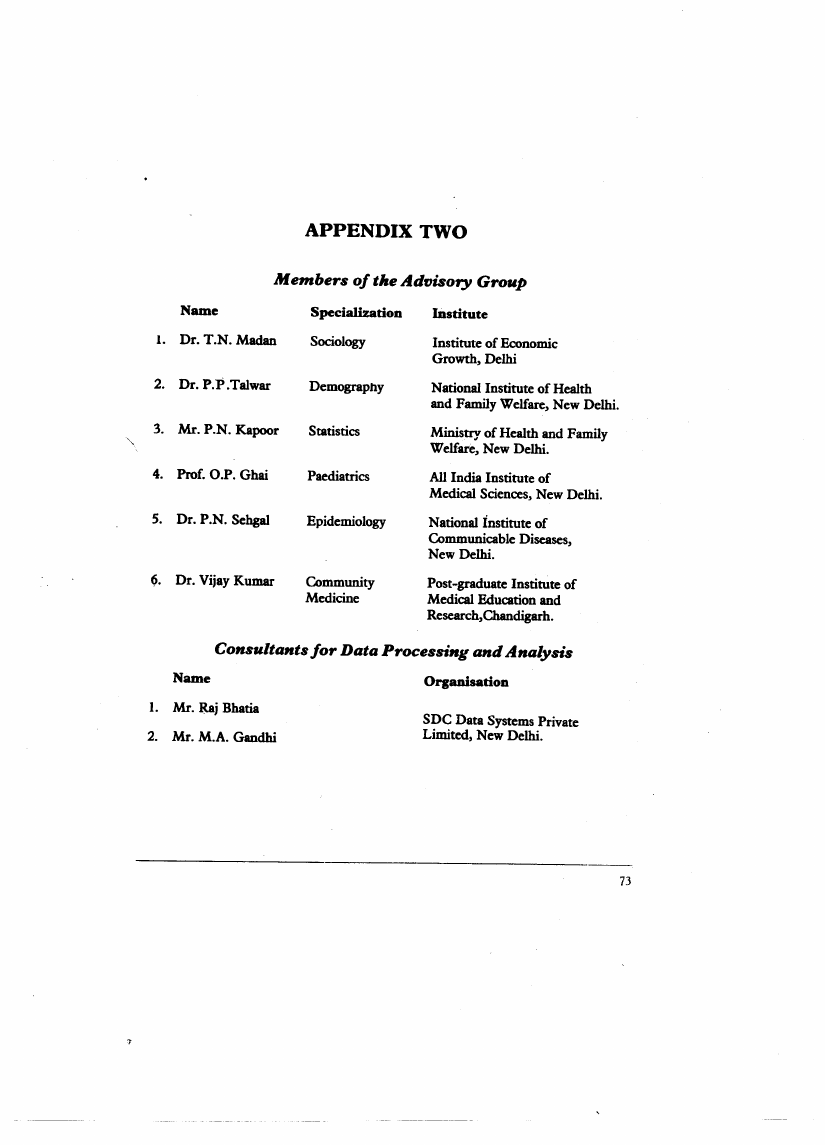
8.3 Page 73 |
▲back to top |

 |
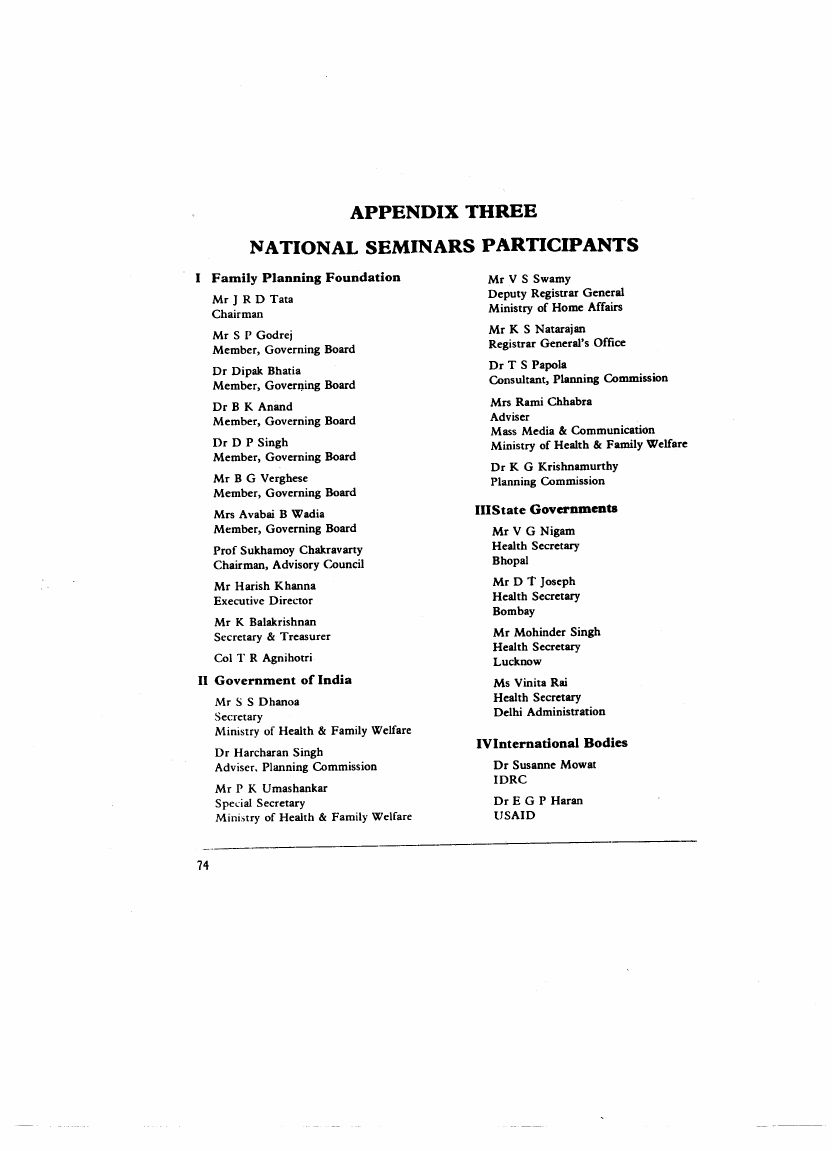
8.4 Page 74 |
▲back to top |

 |
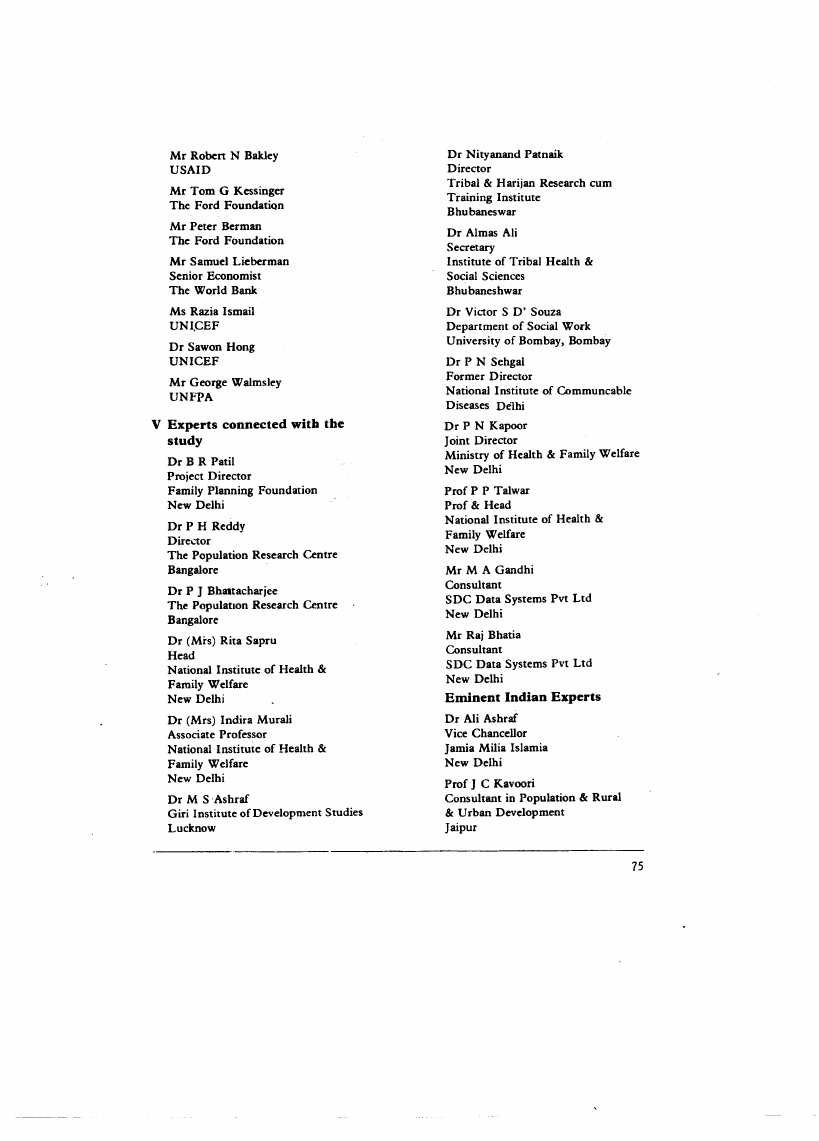
8.5 Page 75 |
▲back to top |
 |
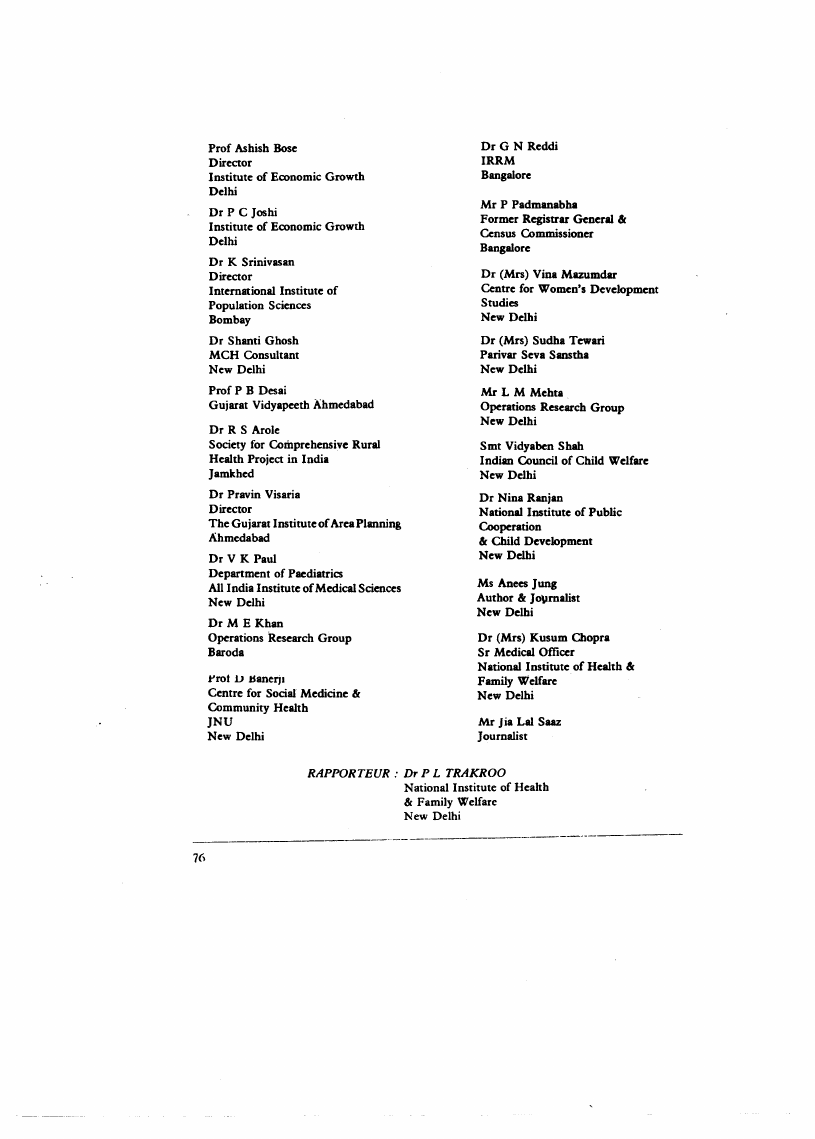
8.6 Page 76 |
▲back to top |
 |
8.7 Page 77 |
▲back to top |
 |
8.8 Page 78 |
▲back to top |
 |
8.9 Page 79 |
▲back to top |
 |
8.10 Page 80 |
▲back to top |
 |
9 Pages 81-90 |
▲back to top |
 |
9.1 Page 81 |
▲back to top |
 |
9.2 Page 82 |
▲back to top |
 |
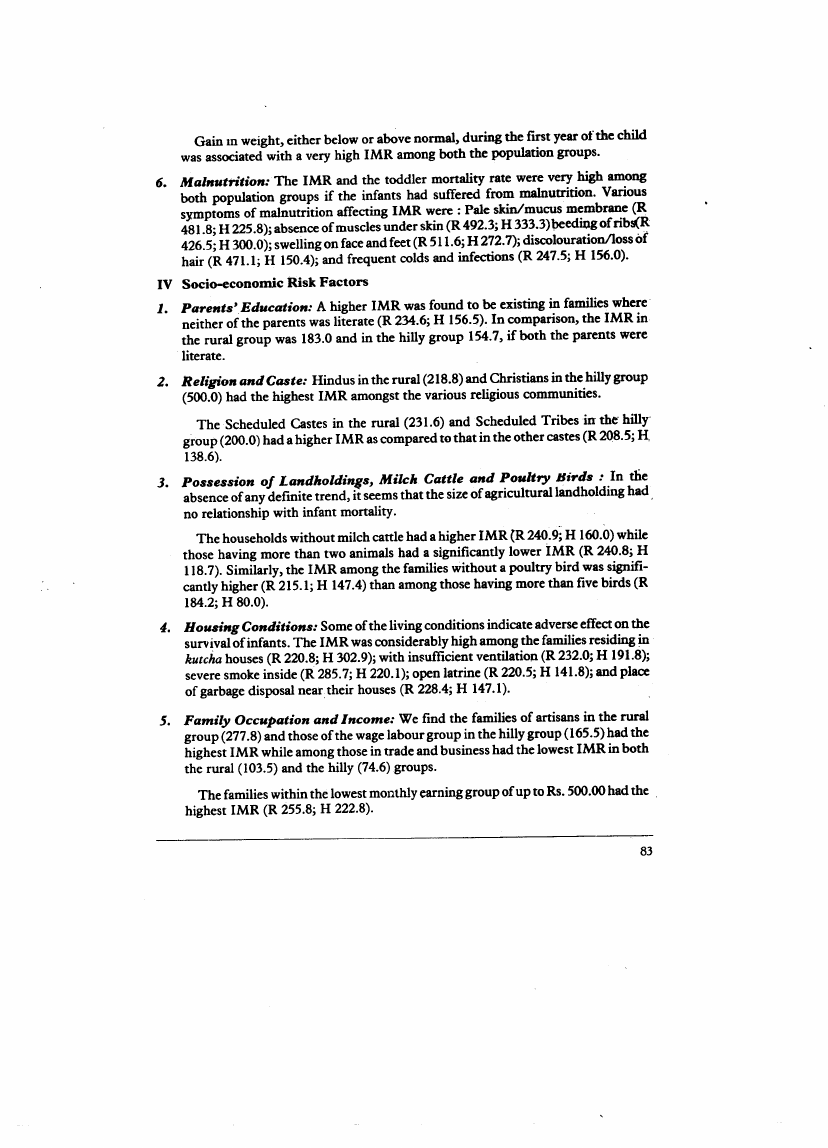
9.3 Page 83 |
▲back to top |
 |
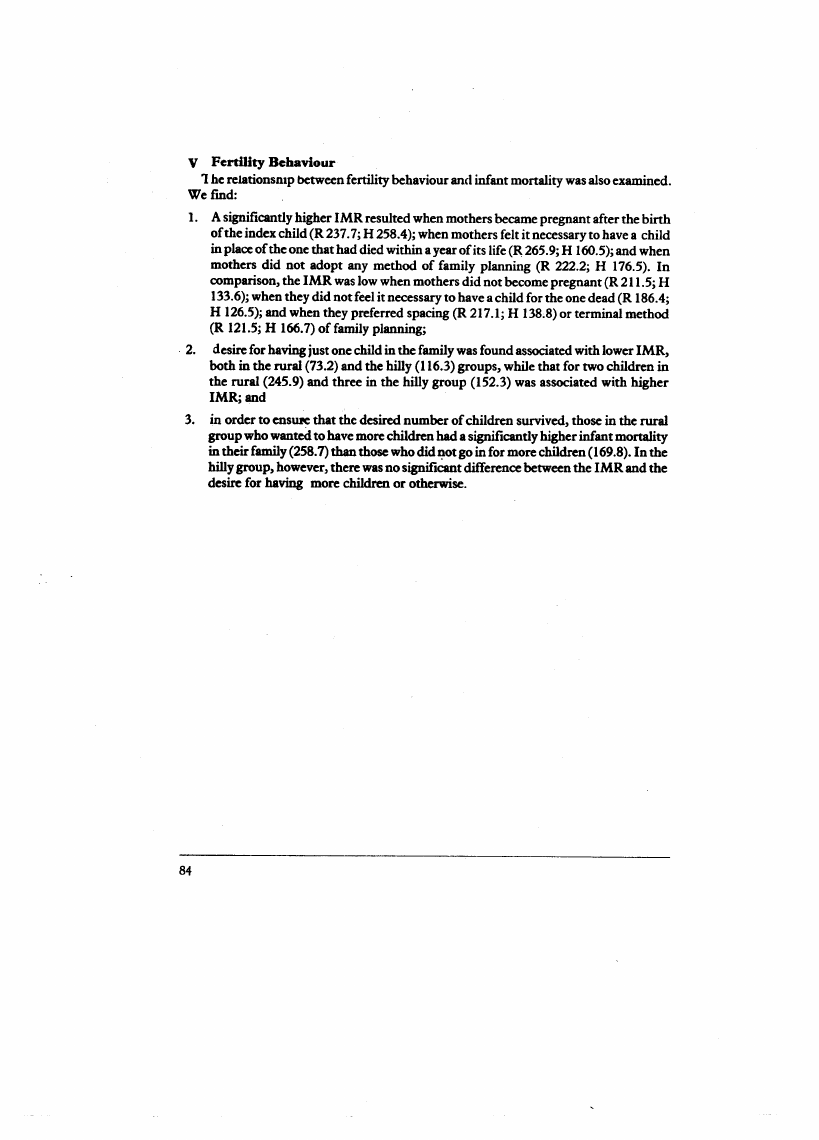
9.4 Page 84 |
▲back to top |
 |
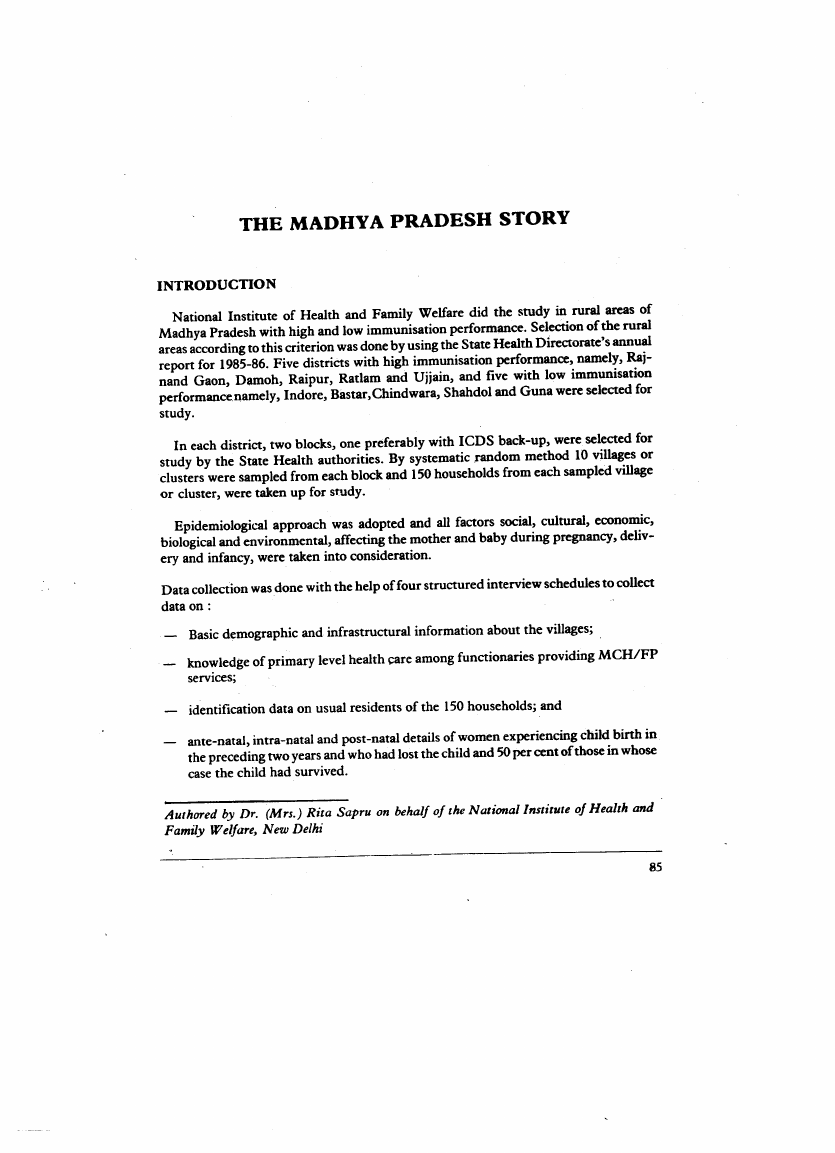
9.5 Page 85 |
▲back to top |
 |
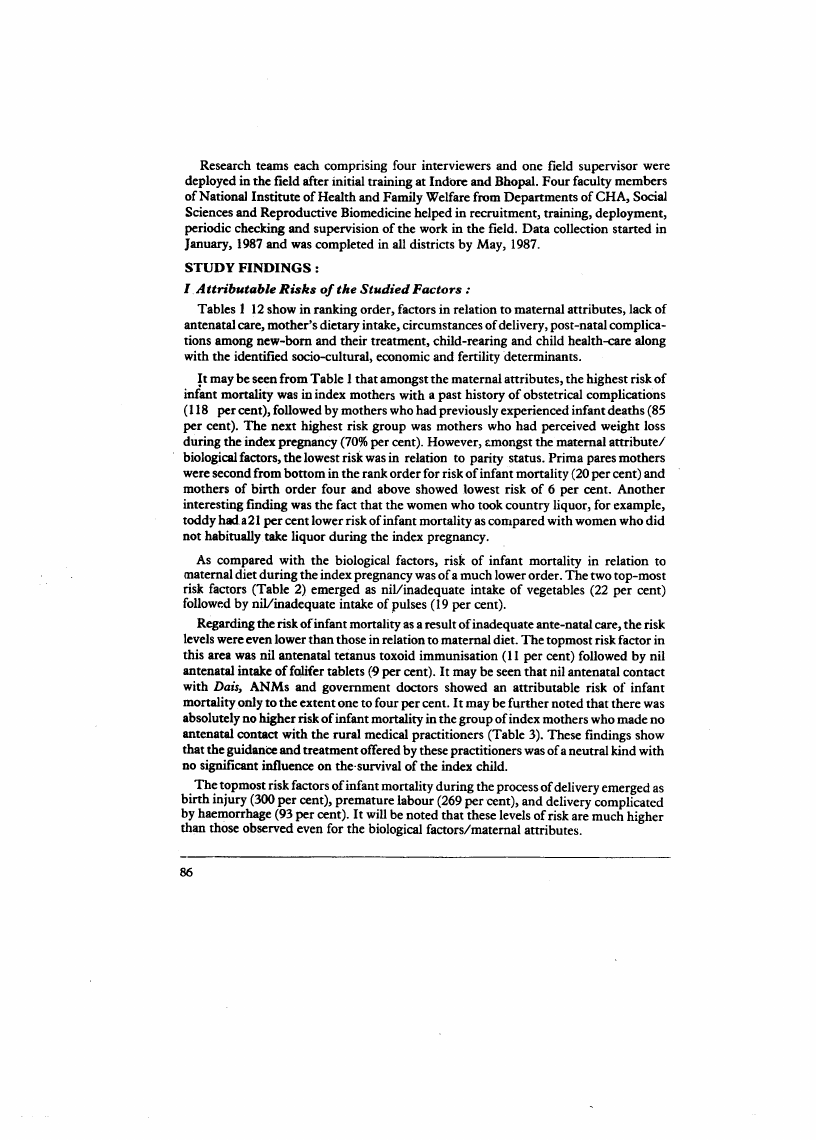
9.6 Page 86 |
▲back to top |
 |
9.7 Page 87 |
▲back to top |
 |
9.8 Page 88 |
▲back to top |

 |
9.9 Page 89 |
▲back to top |
 |
9.10 Page 90 |
▲back to top |
 |
10 Pages 91-100 |
▲back to top |
 |
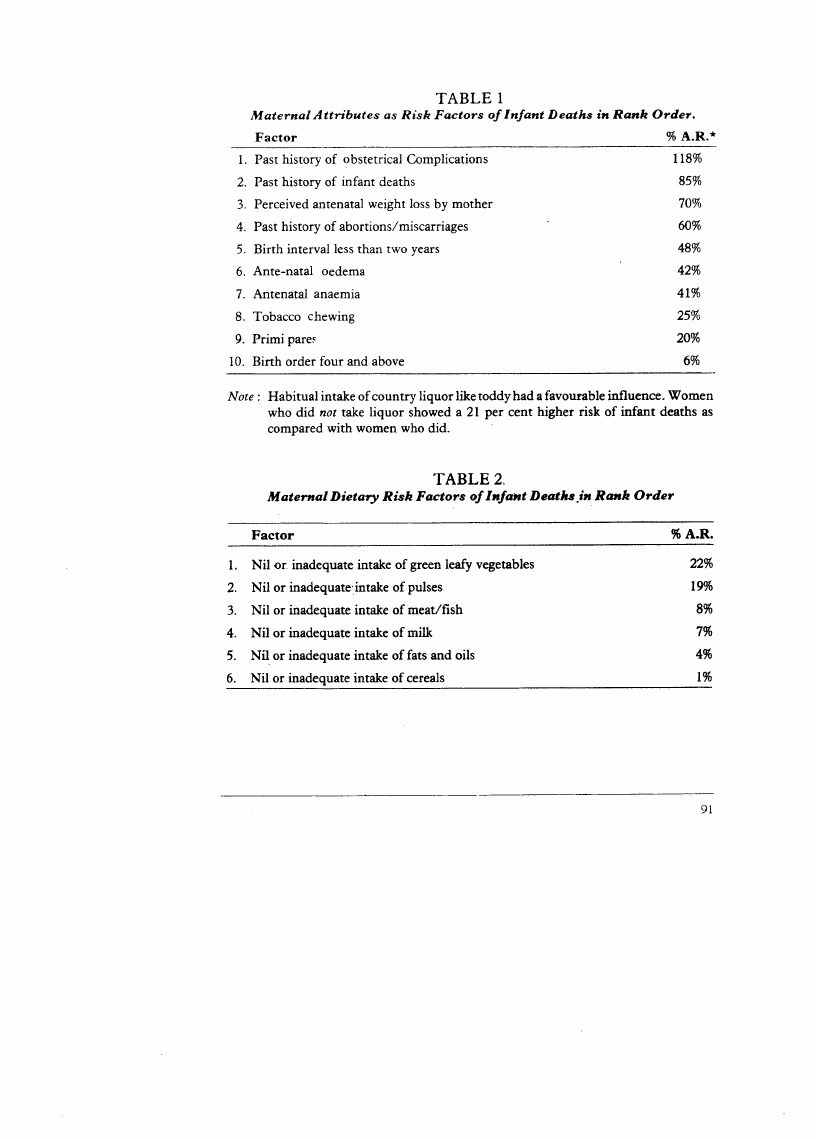
10.1 Page 91 |
▲back to top |
 |
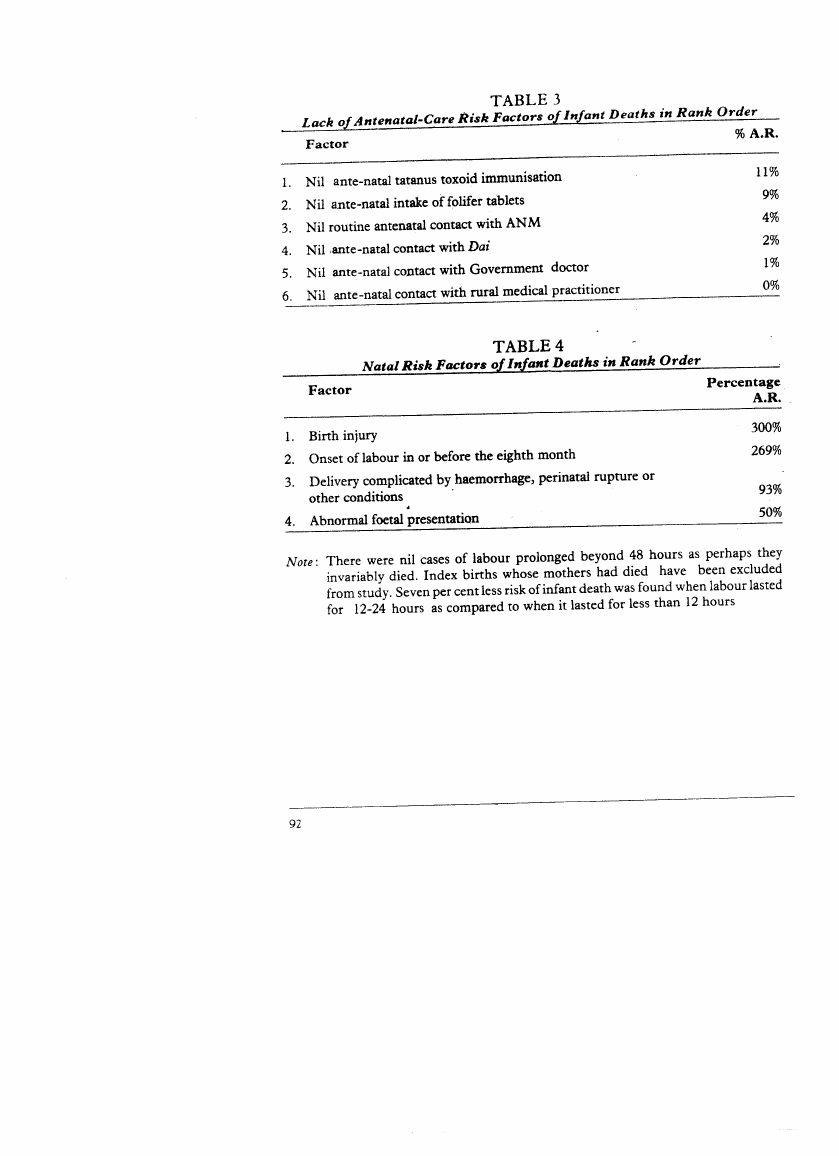
10.2 Page 92 |
▲back to top |
 |
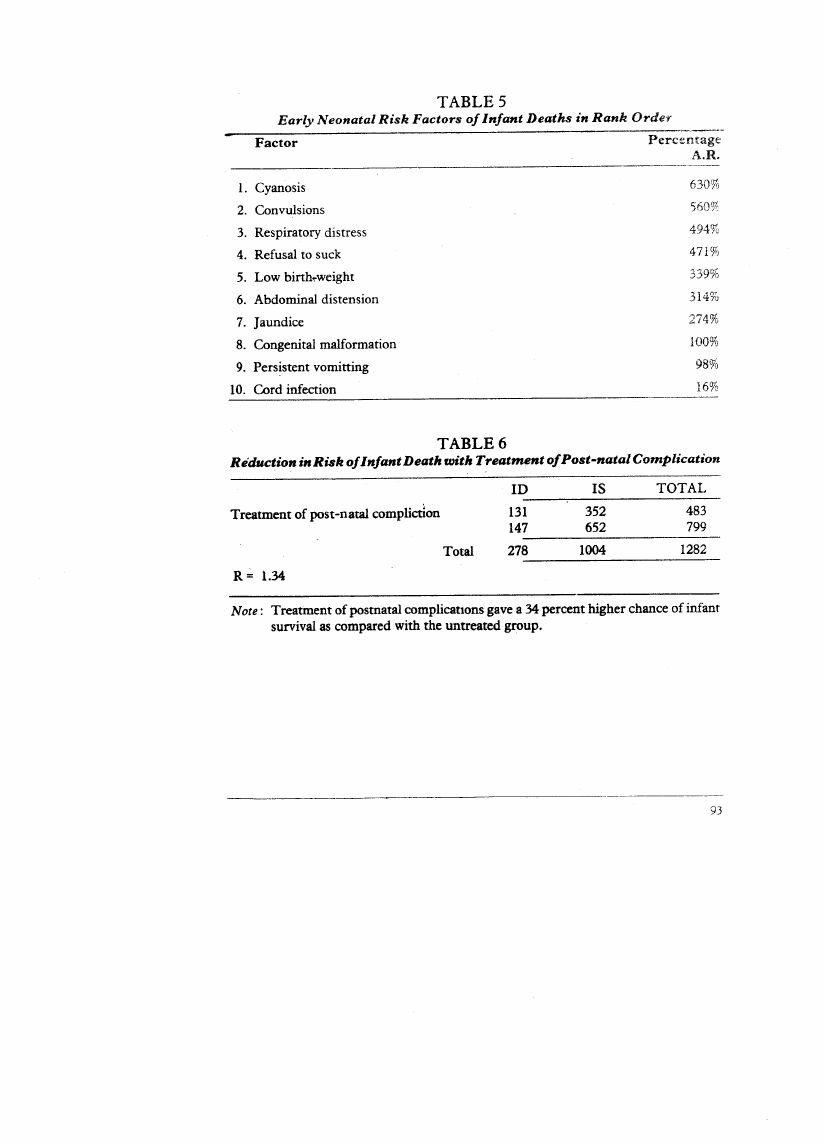
10.3 Page 93 |
▲back to top |
 |
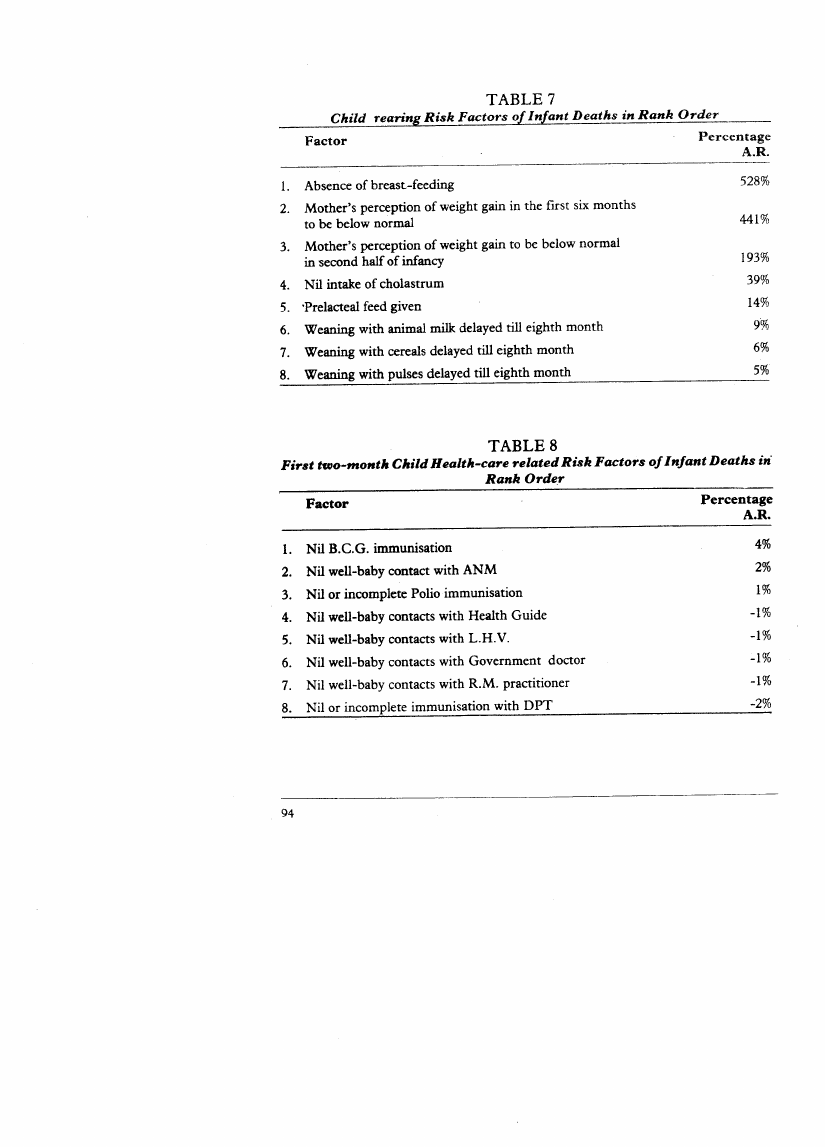
10.4 Page 94 |
▲back to top |
 |
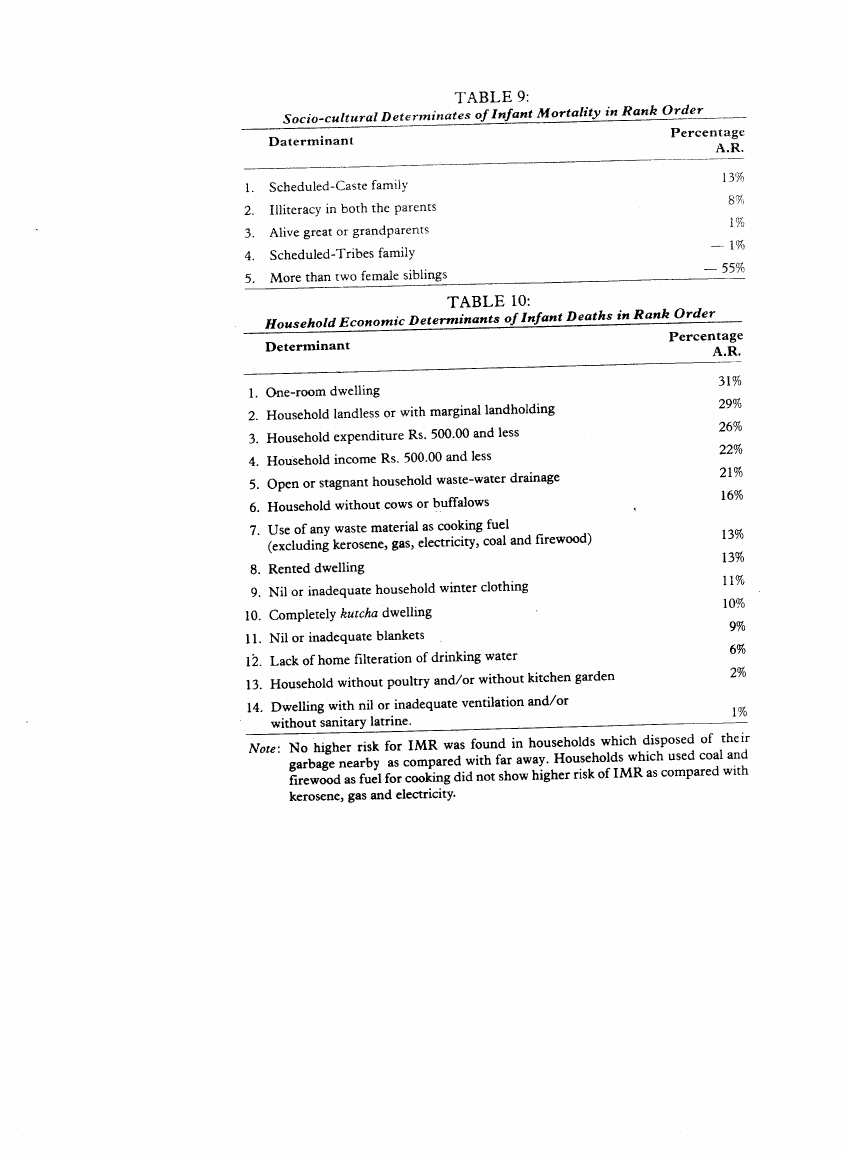
10.5 Page 95 |
▲back to top |
 |
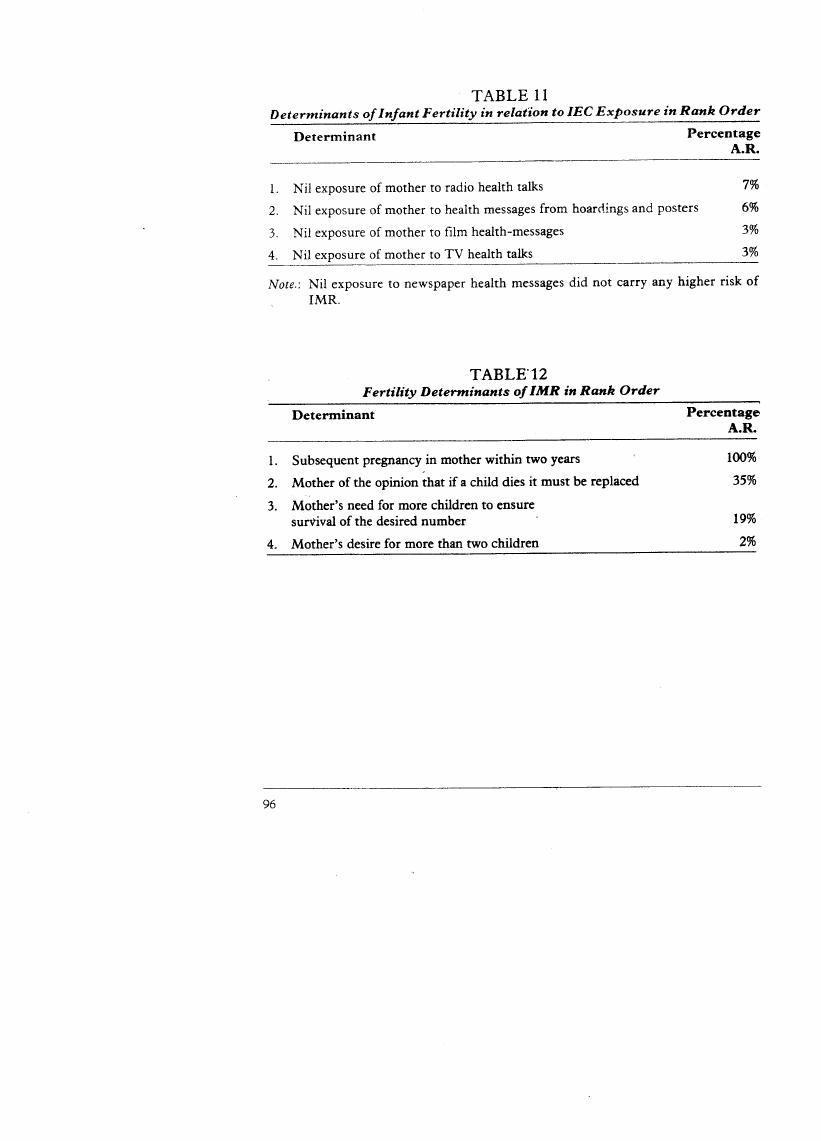
10.6 Page 96 |
▲back to top |
 |
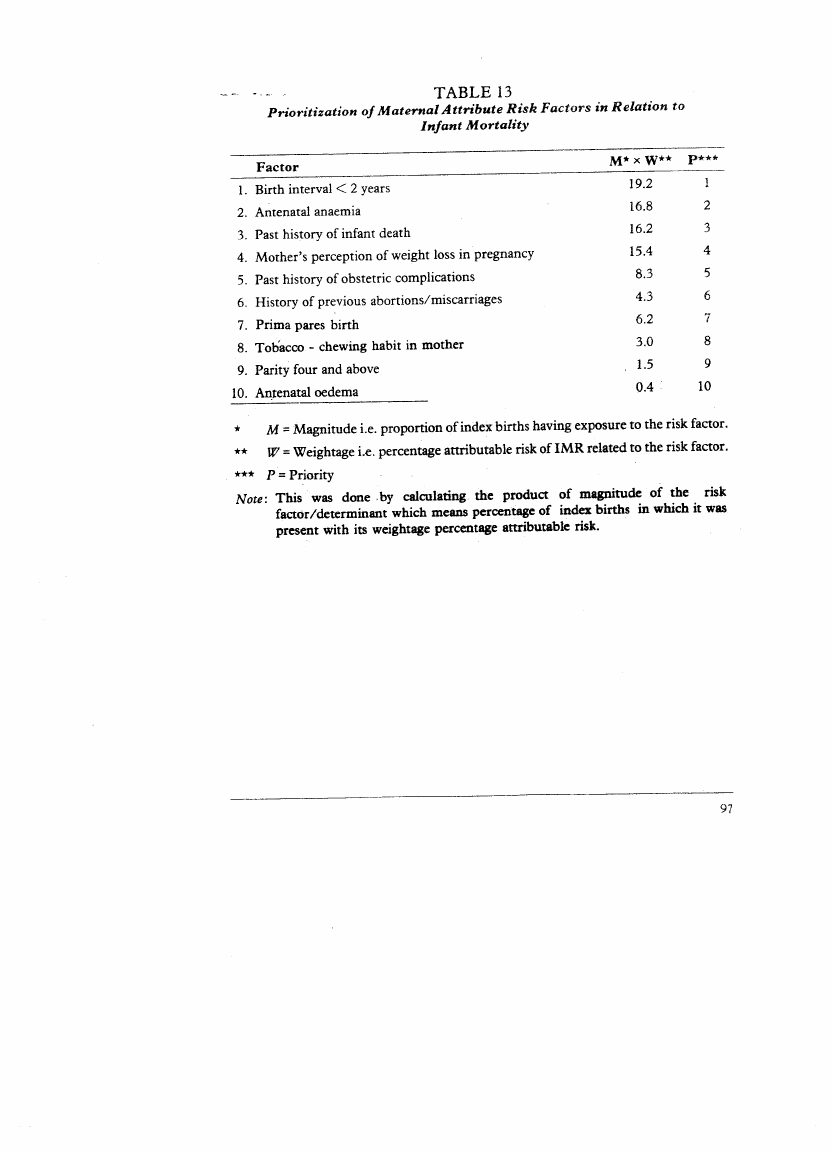
10.7 Page 97 |
▲back to top |
 |
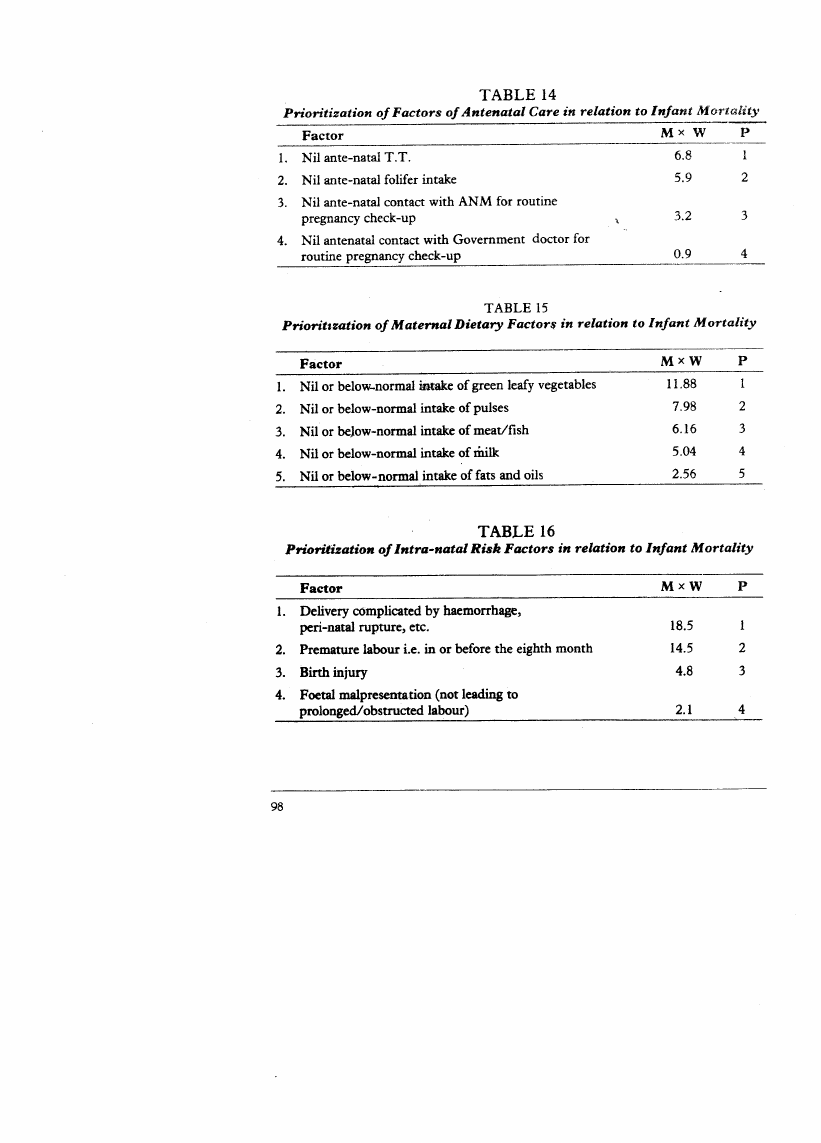
10.8 Page 98 |
▲back to top |
 |
10.9 Page 99 |
▲back to top |
 |
10.10 Page 100 |
▲back to top |
 |
11 Pages 101-110 |
▲back to top |
 |
11.1 Page 101 |
▲back to top |
 |
11.2 Page 102 |
▲back to top |
 |
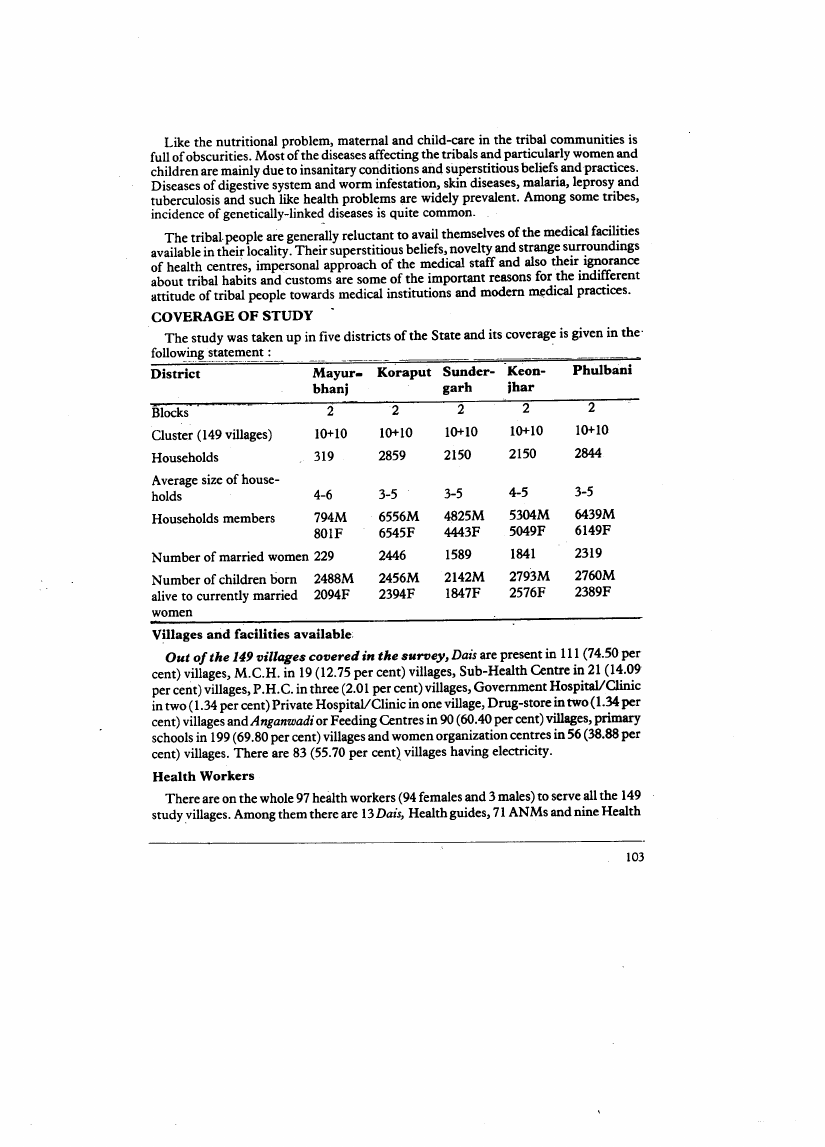
11.3 Page 103 |
▲back to top |
 |
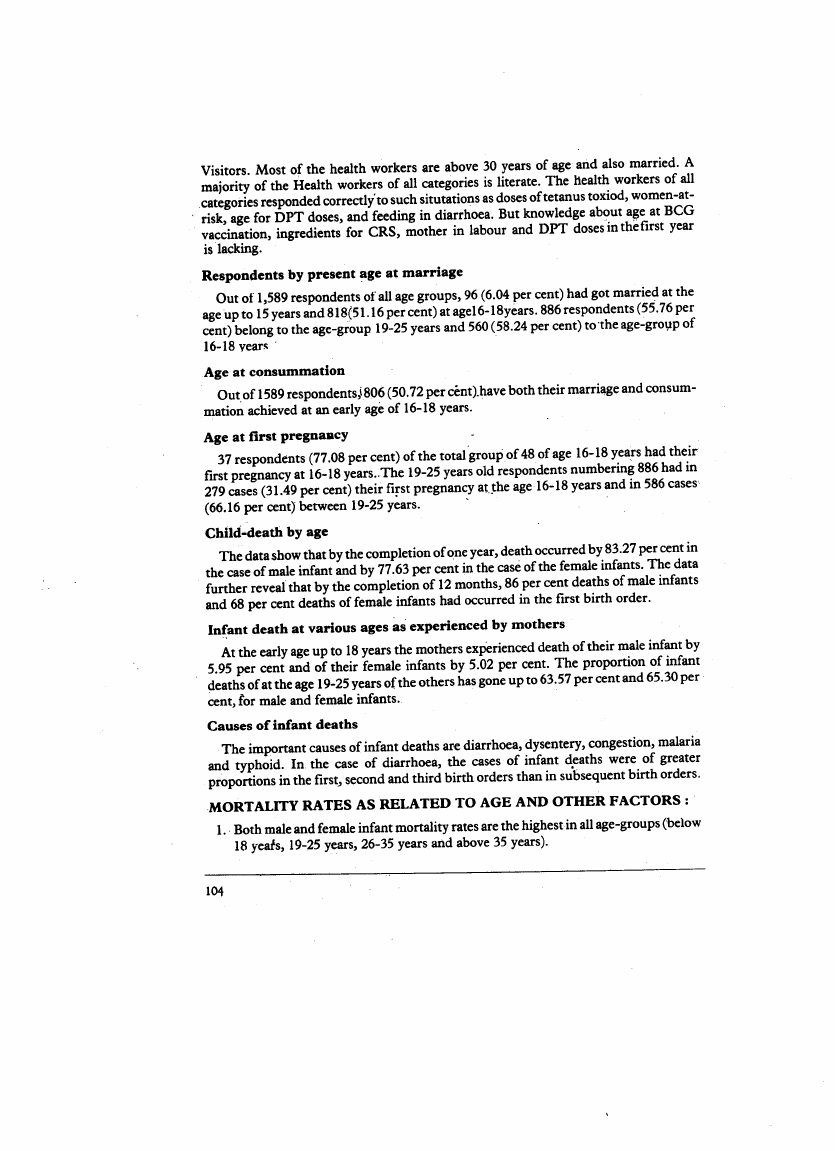
11.4 Page 104 |
▲back to top |
 |
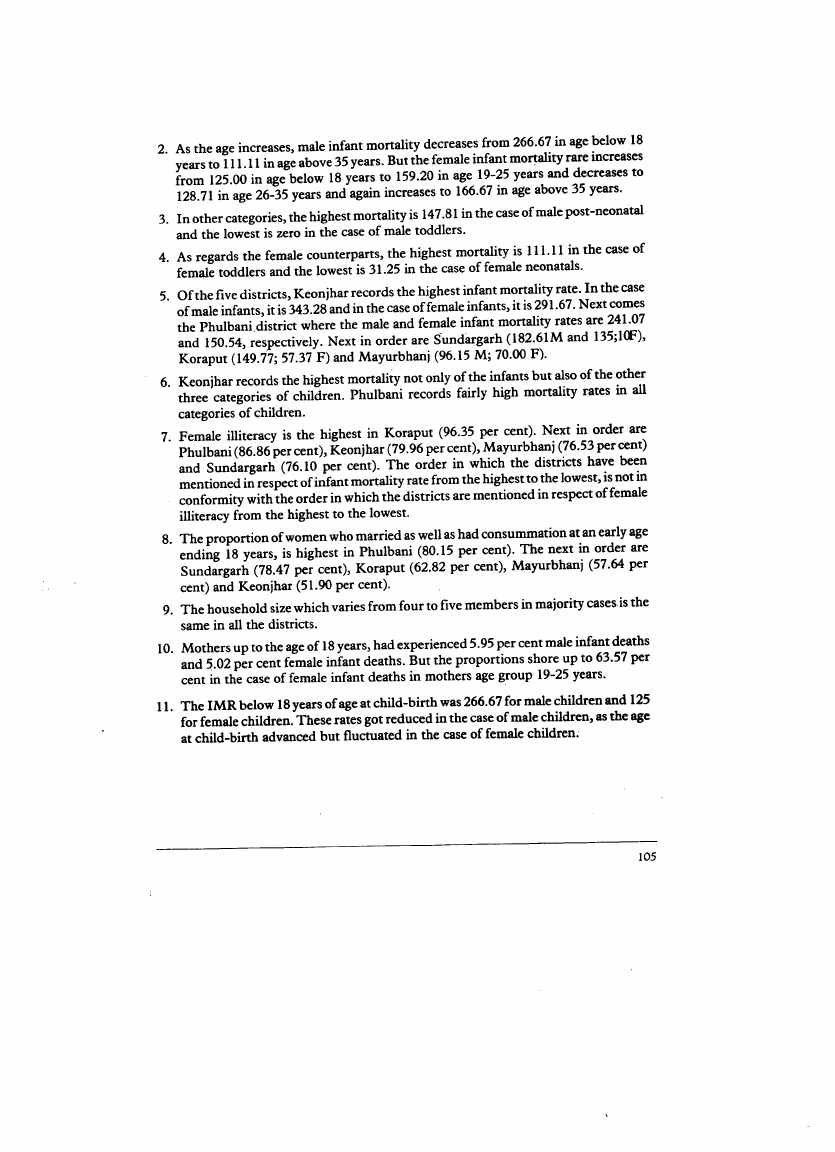
11.5 Page 105 |
▲back to top |
 |
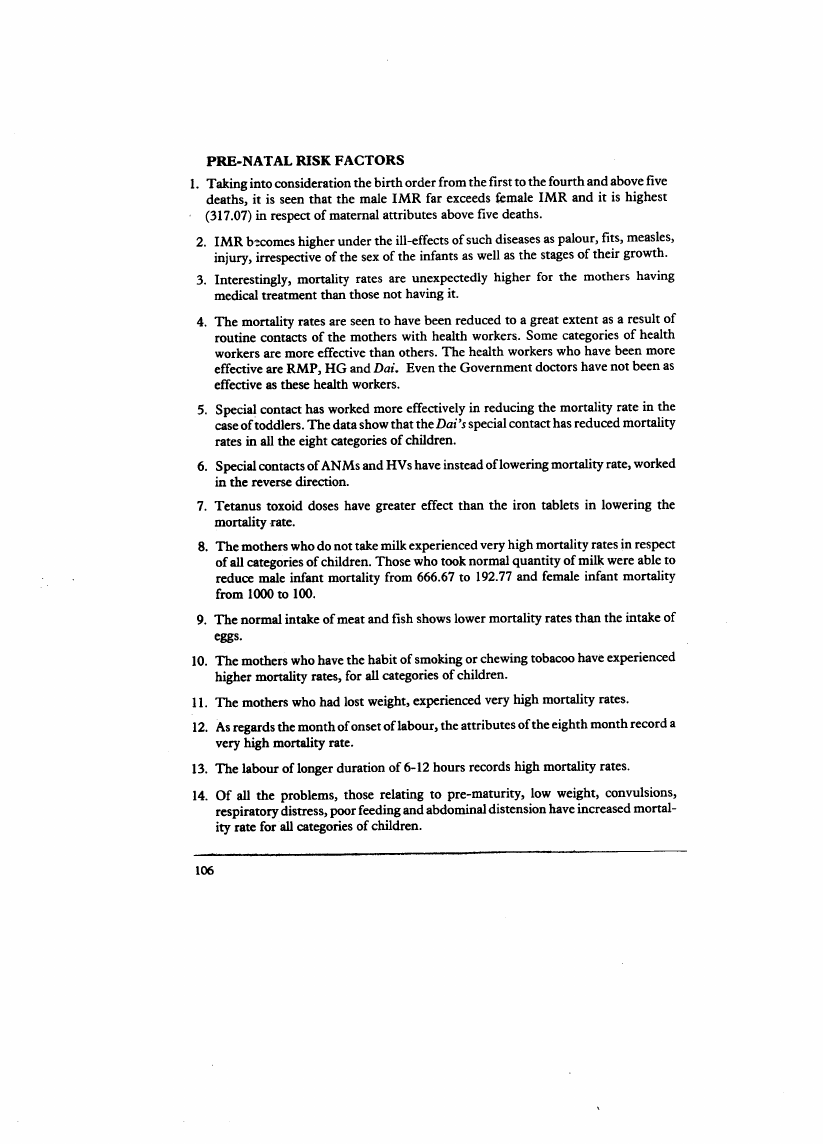
11.6 Page 106 |
▲back to top |
 |
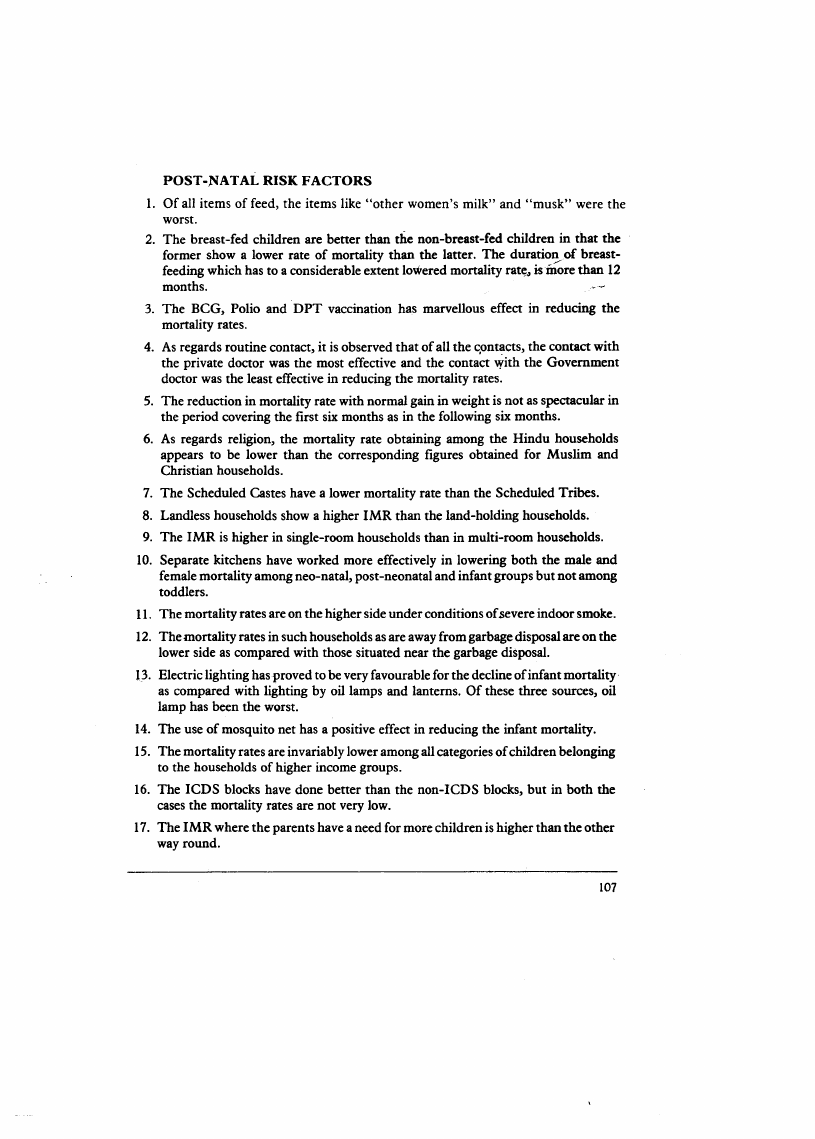
11.7 Page 107 |
▲back to top |
 |
11.8 Page 108 |
▲back to top |
 |
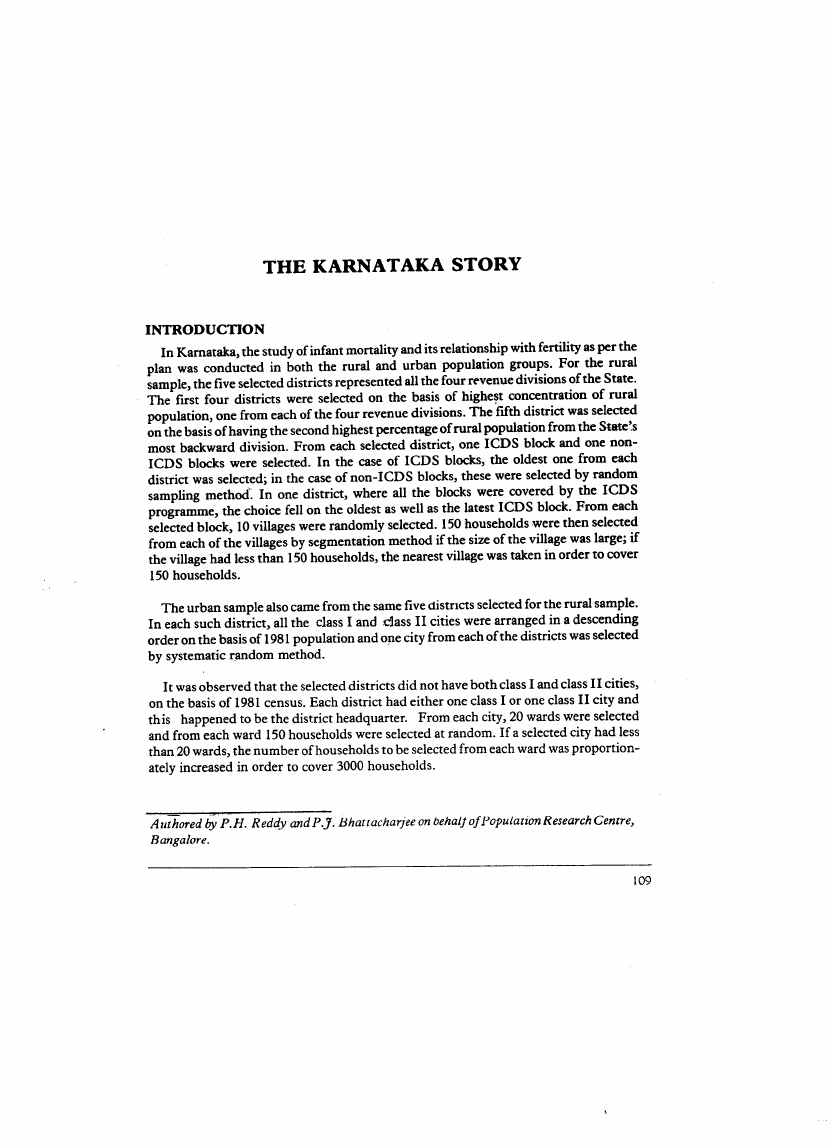
11.9 Page 109 |
▲back to top |
 |
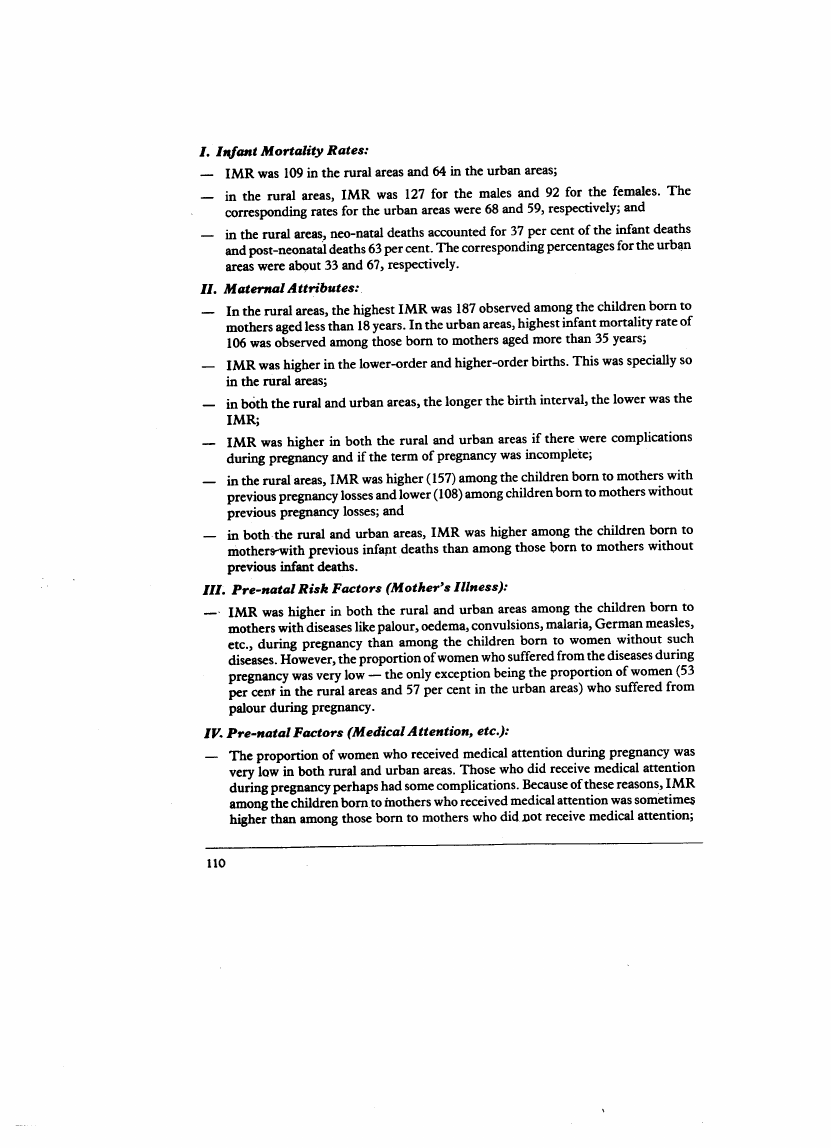
11.10 Page 110 |
▲back to top |
 |
12 Pages 111-120 |
▲back to top |
 |
12.1 Page 111 |
▲back to top |
 |
12.2 Page 112 |
▲back to top |
 |
12.3 Page 113 |
▲back to top |
 |
12.4 Page 114 |
▲back to top |
 |
12.5 Page 115 |
▲back to top |
 |
12.6 Page 116 |
▲back to top |
 |
12.7 Page 117 |
▲back to top |
 |
12.8 Page 118 |
▲back to top |
 |
12.9 Page 119 |
▲back to top |
 |
12.10 Page 120 |
▲back to top |
 |
13 Pages 121-130 |
▲back to top |
 |
13.1 Page 121 |
▲back to top |
 |
13.2 Page 122 |
▲back to top |
 |
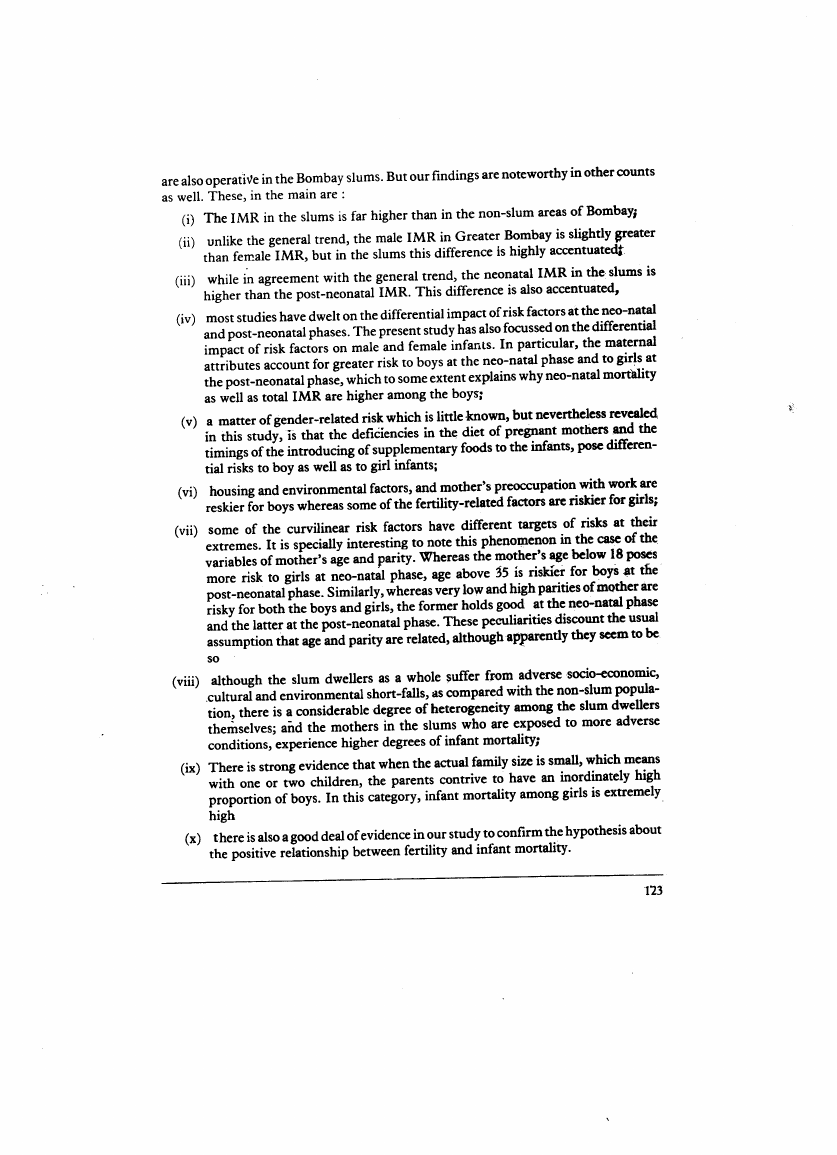
13.3 Page 123 |
▲back to top |
 |
13.4 Page 124 |
▲back to top |
 |
13.5 Page 125 |
▲back to top |
 |
13.6 Page 126 |
▲back to top |
 |
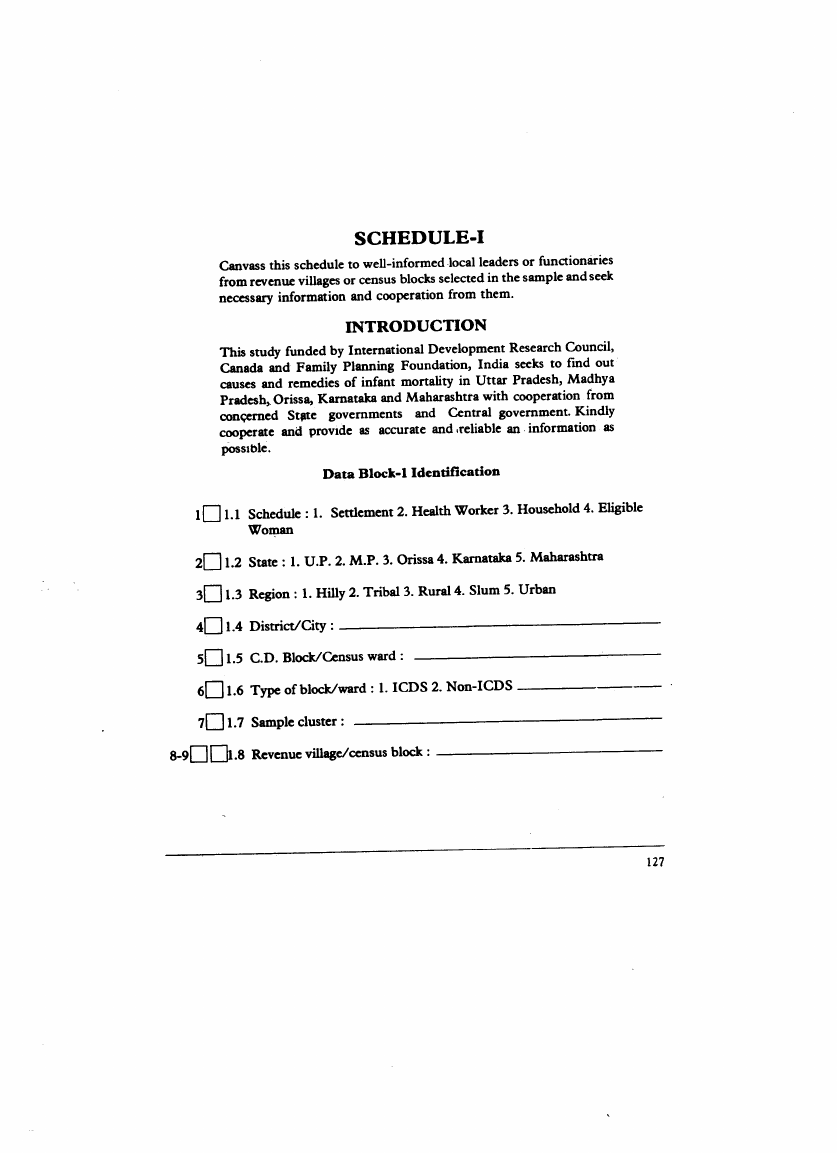
13.7 Page 127 |
▲back to top |
 |
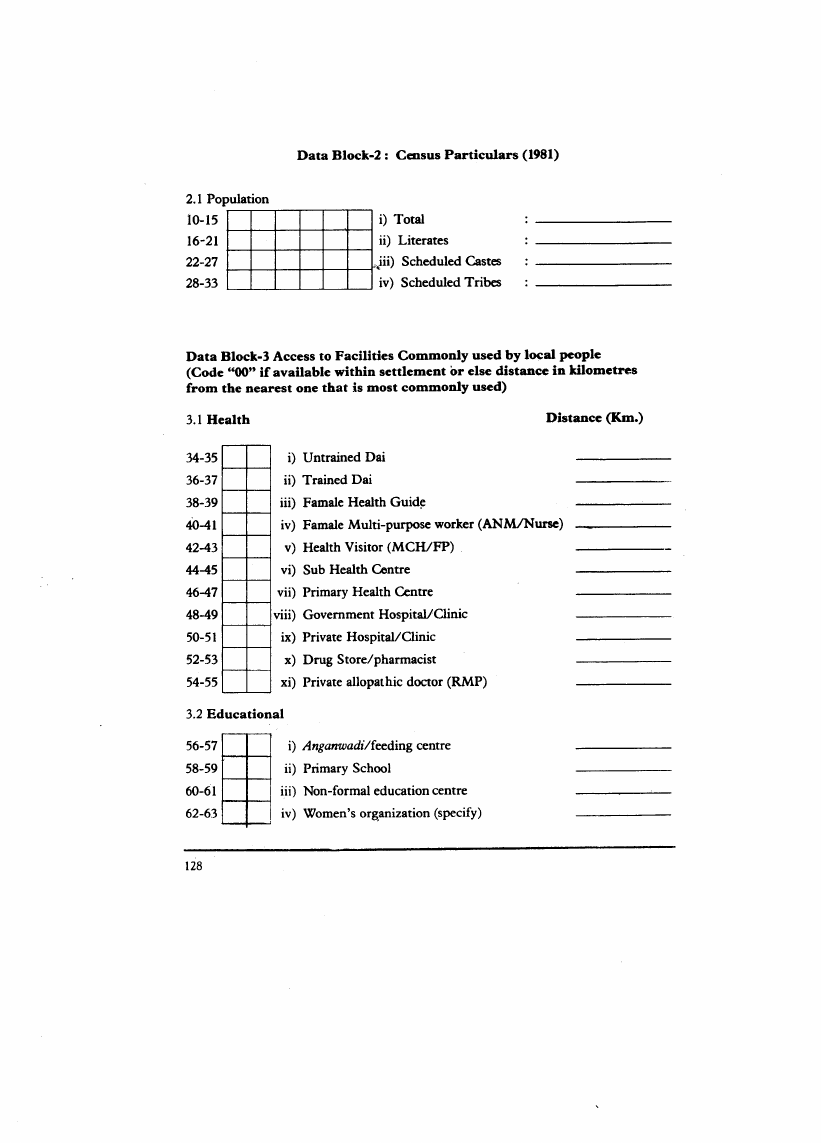
13.8 Page 128 |
▲back to top |
 |
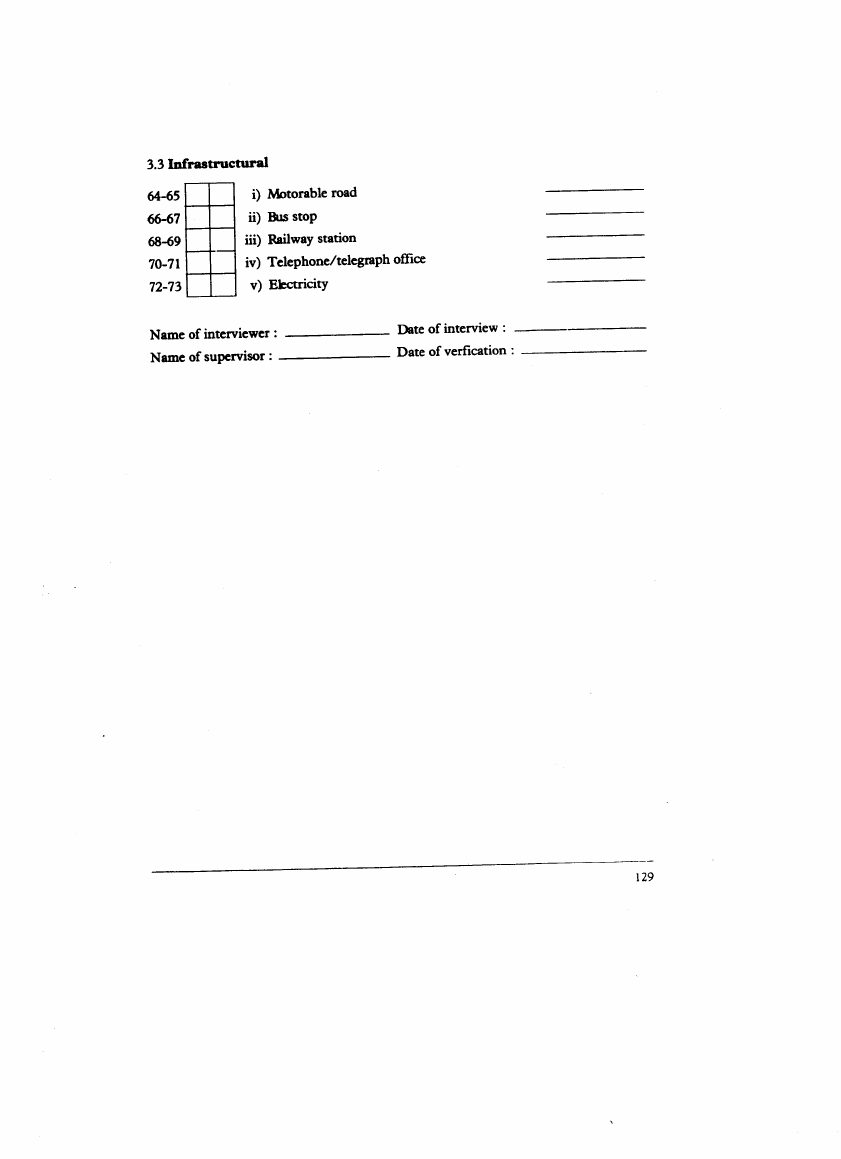
13.9 Page 129 |
▲back to top |
 |
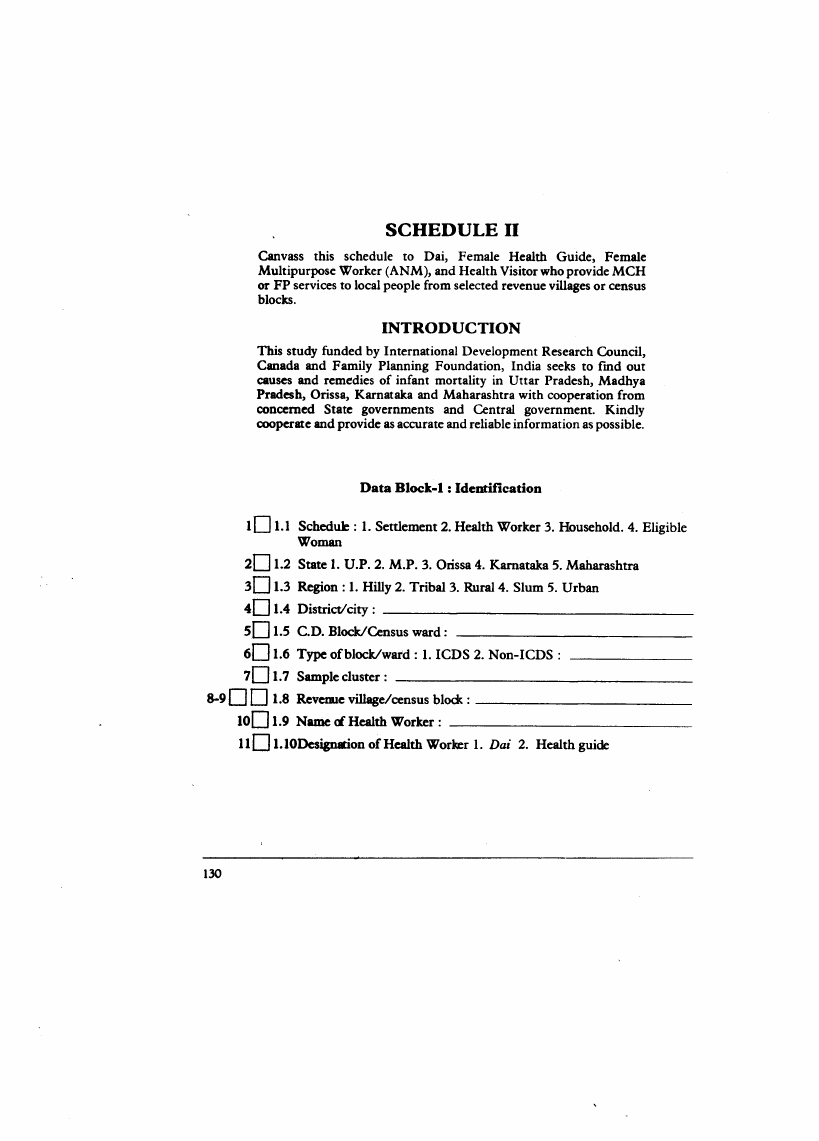
13.10 Page 130 |
▲back to top |
 |
14 Pages 131-140 |
▲back to top |
 |
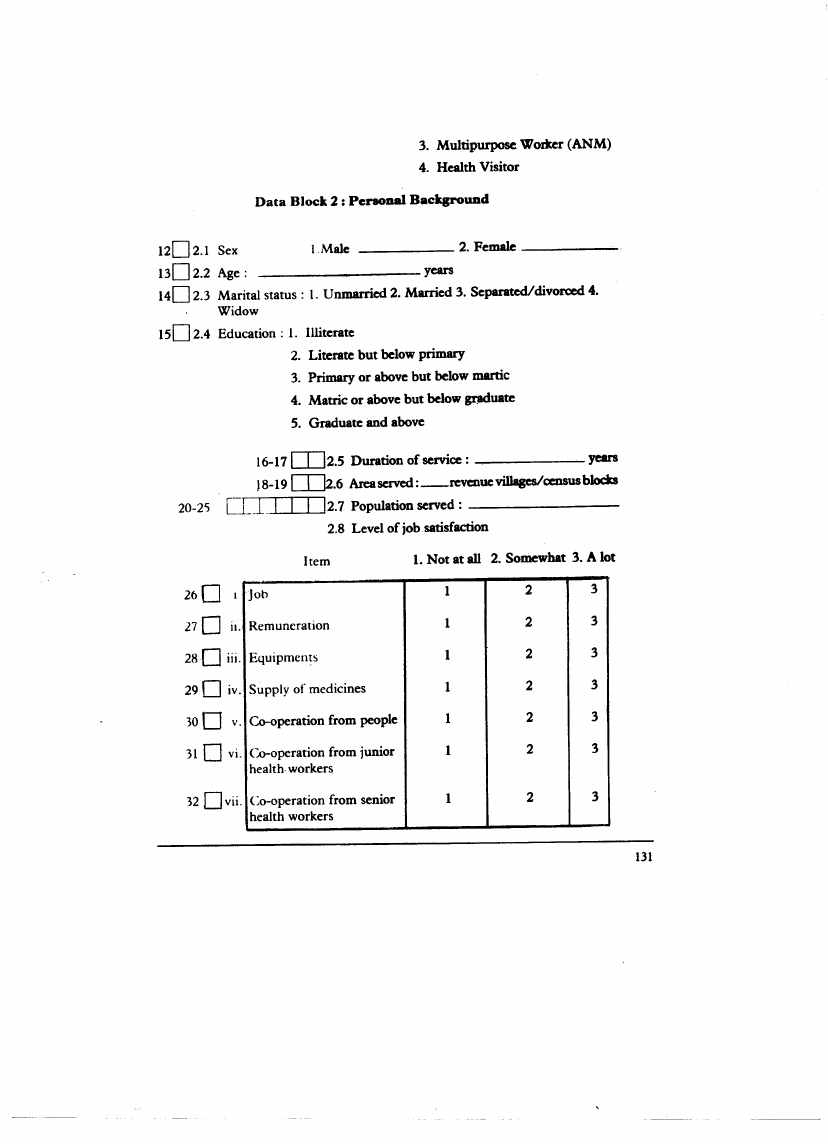
14.1 Page 131 |
▲back to top |
 |
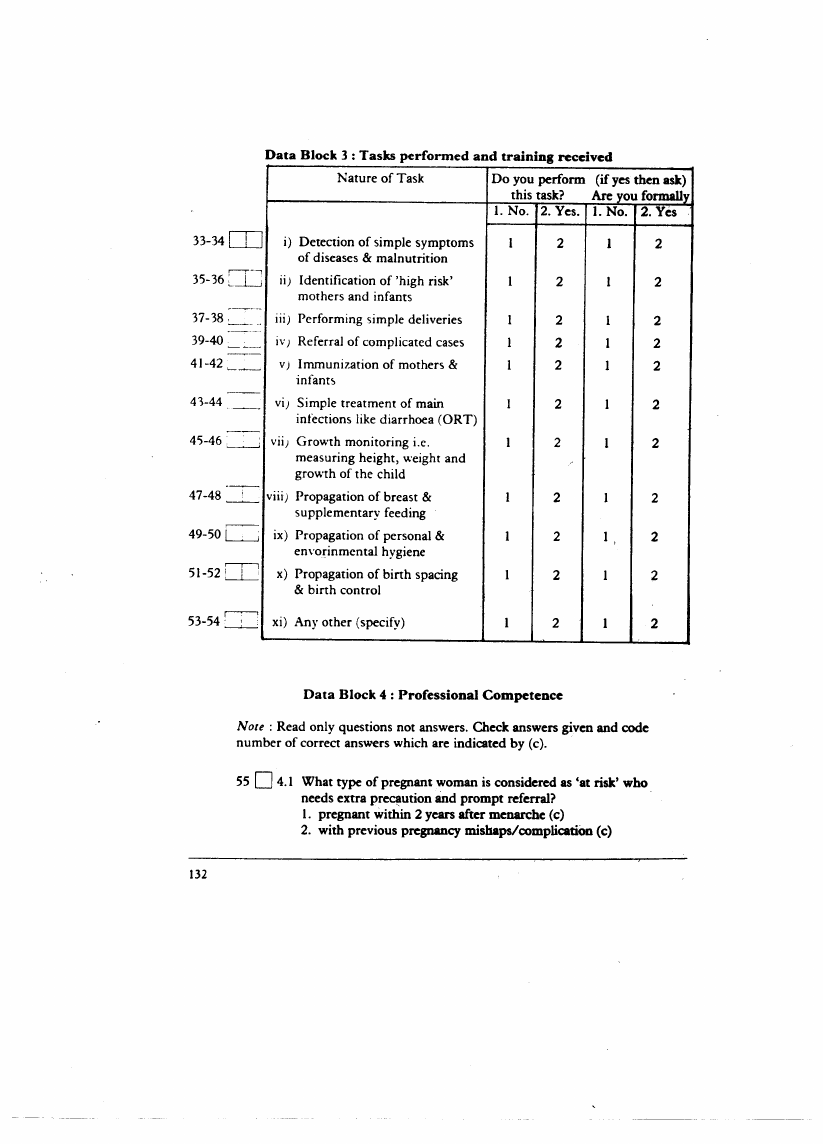
14.2 Page 132 |
▲back to top |
 |
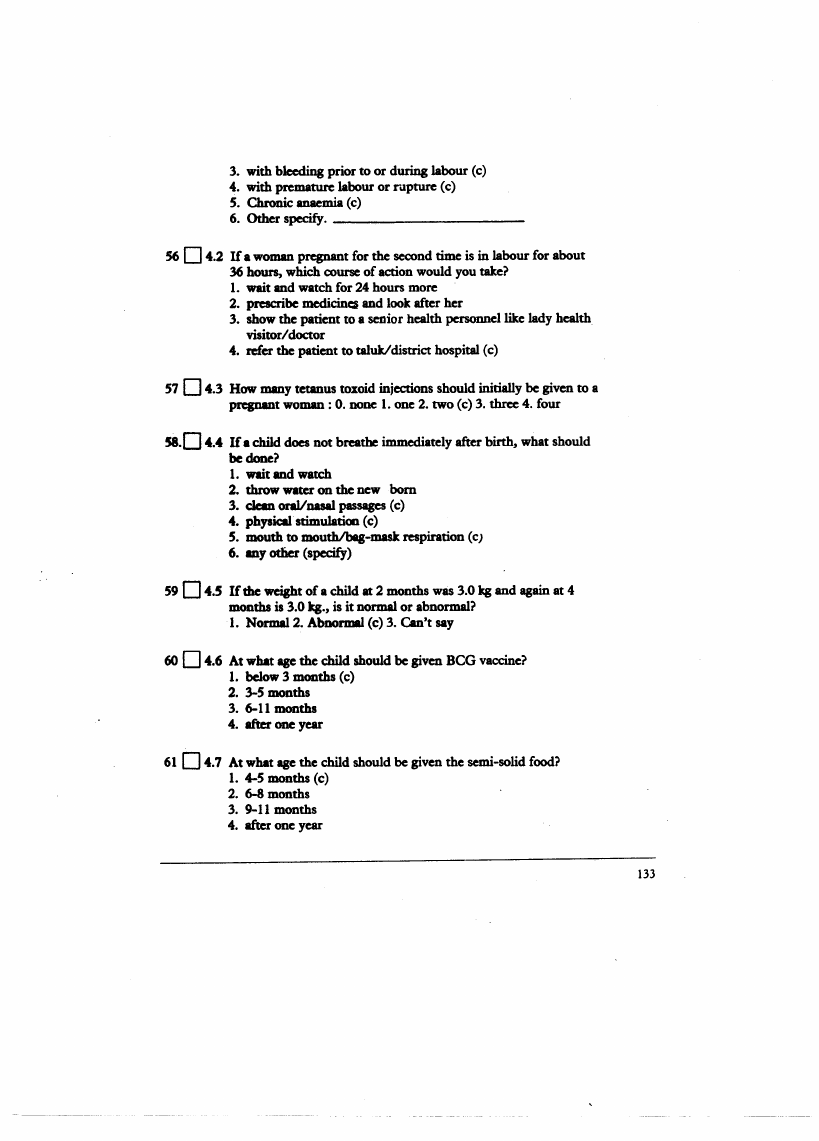
14.3 Page 133 |
▲back to top |
 |
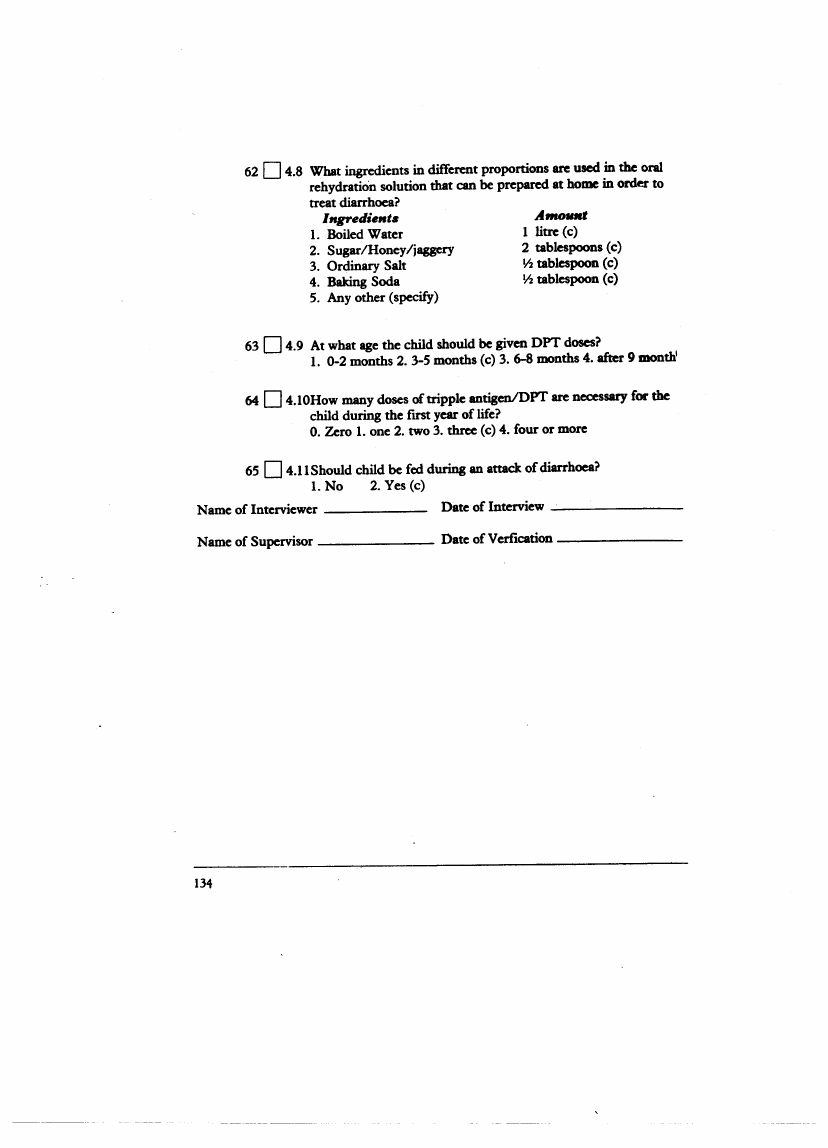
14.4 Page 134 |
▲back to top |
 |
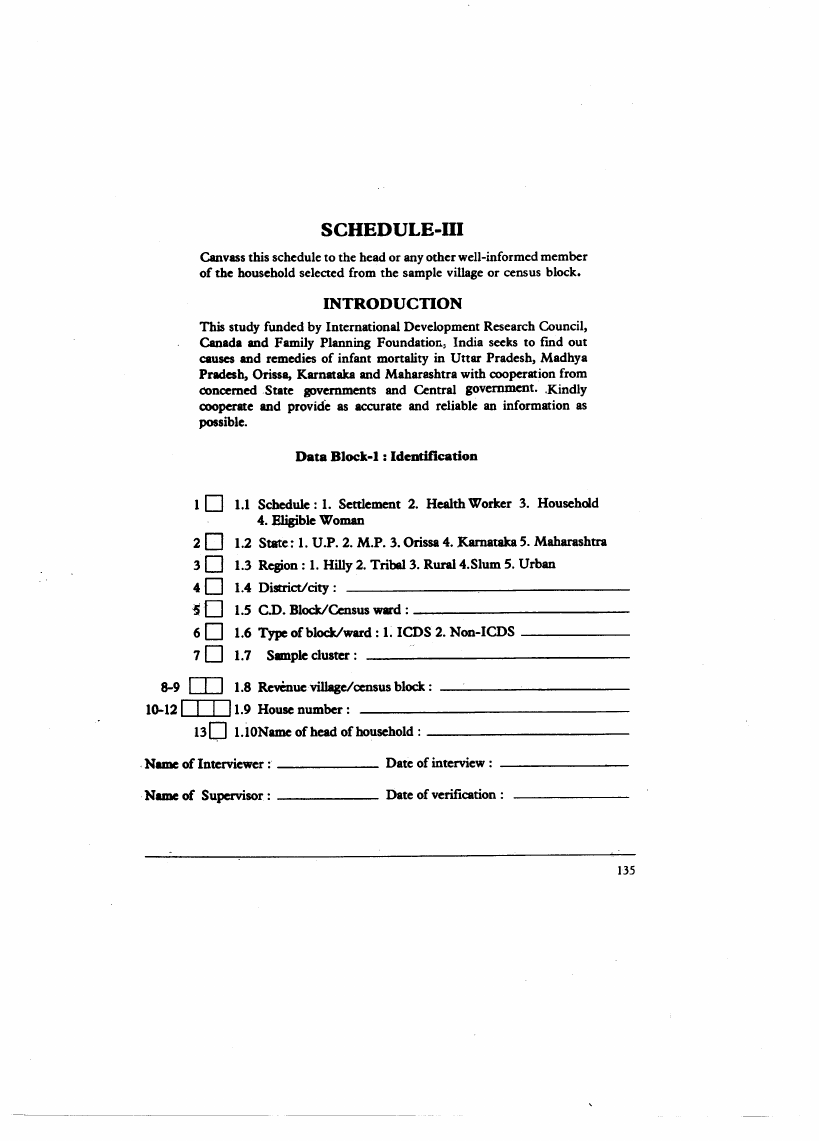
14.5 Page 135 |
▲back to top |
 |
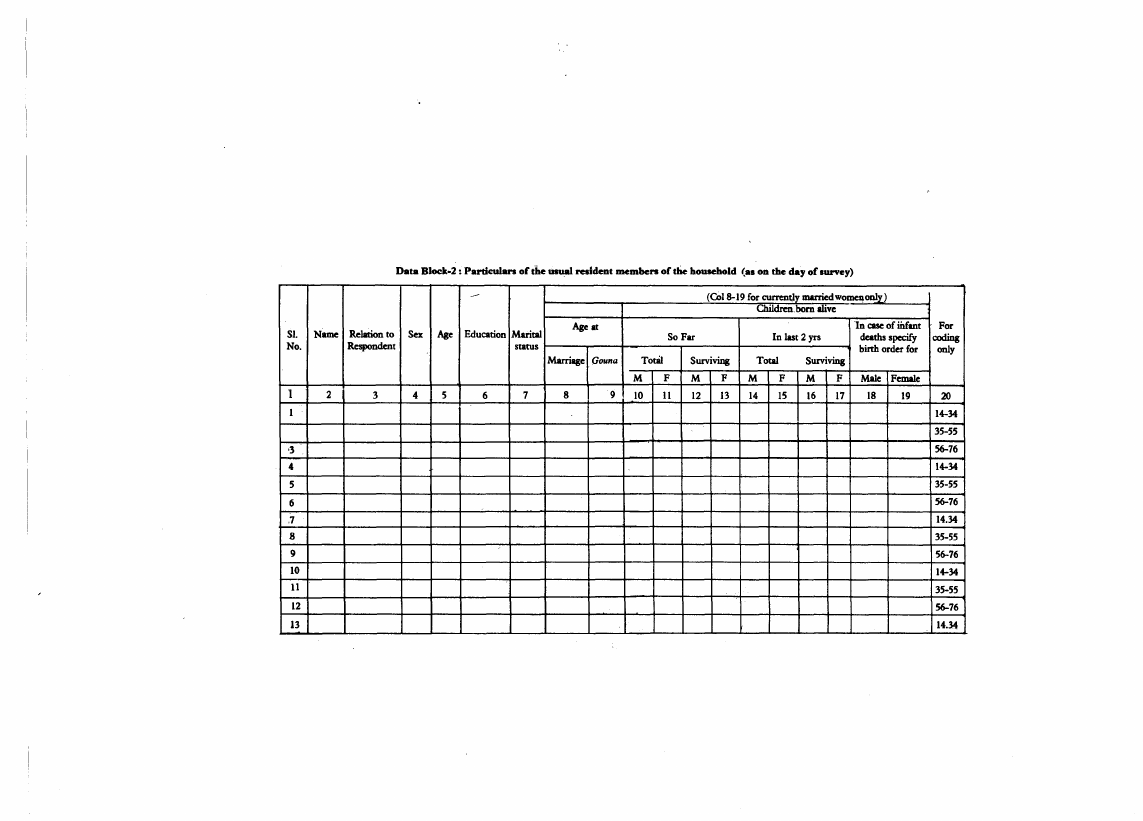
14.6 Page 136 |
▲back to top |
 |
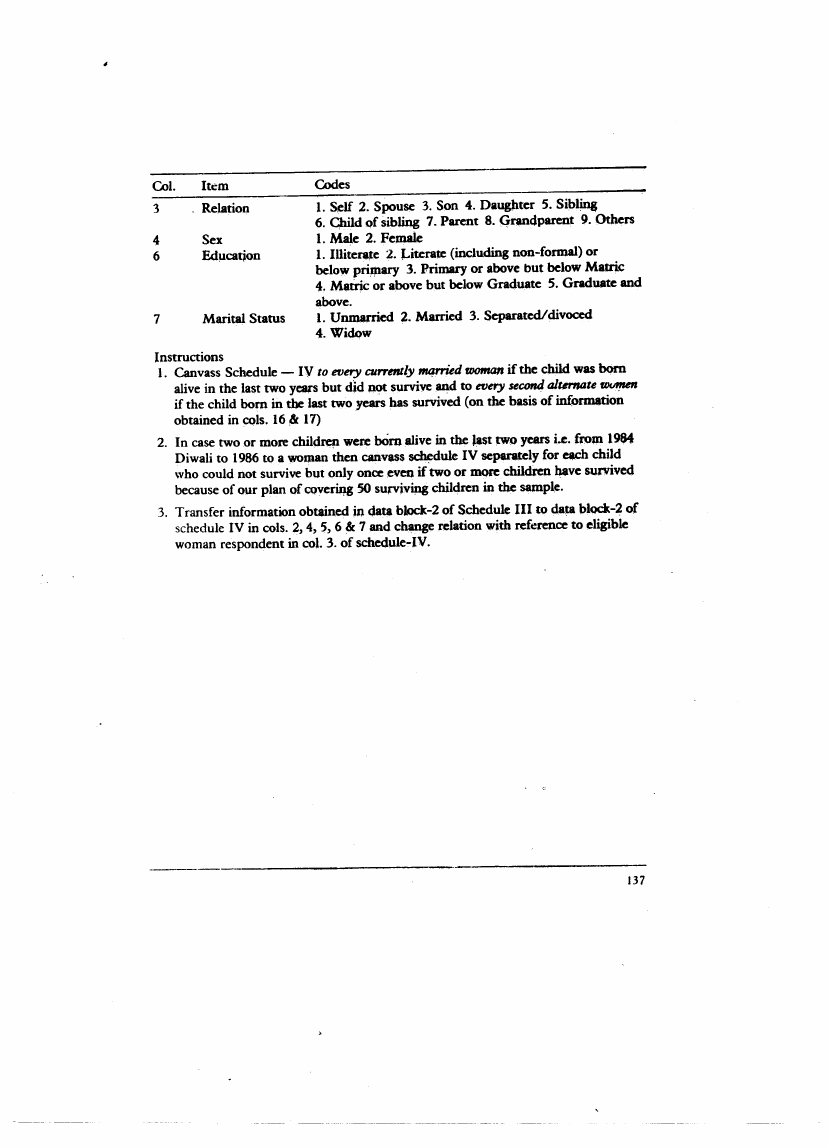
14.7 Page 137 |
▲back to top |
 |
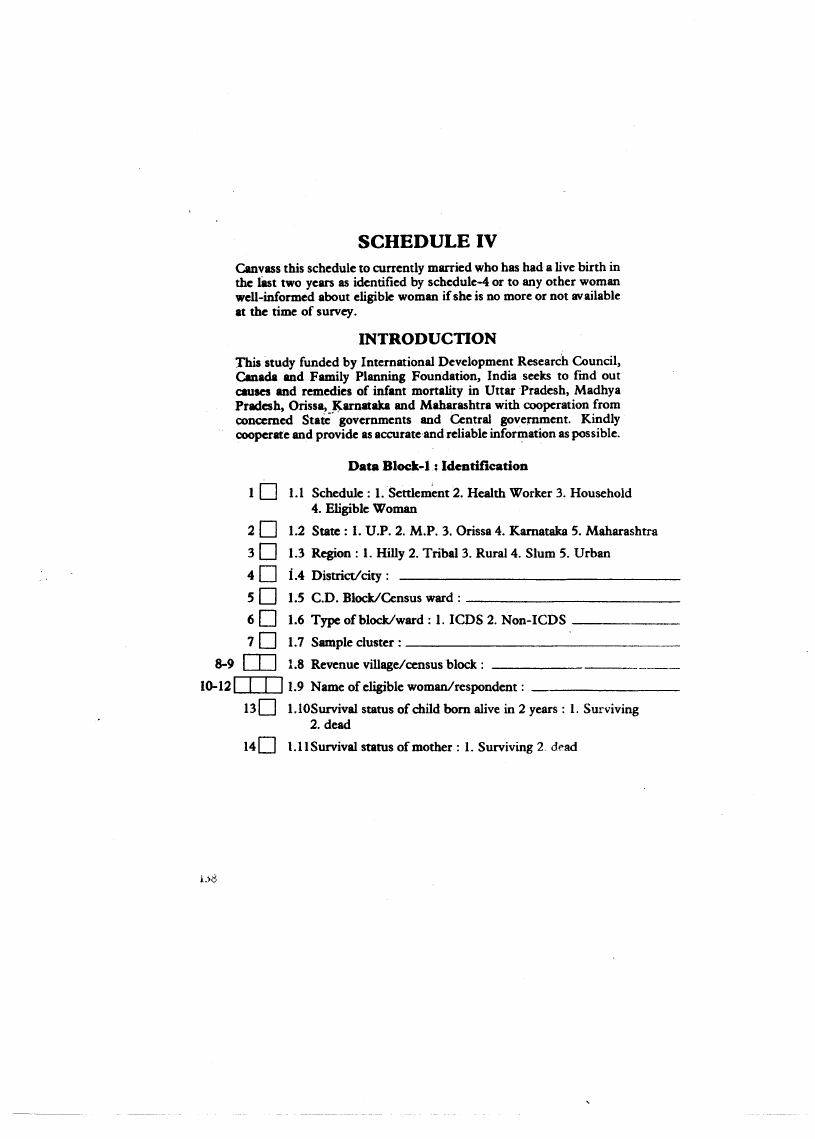
14.8 Page 138 |
▲back to top |
 |
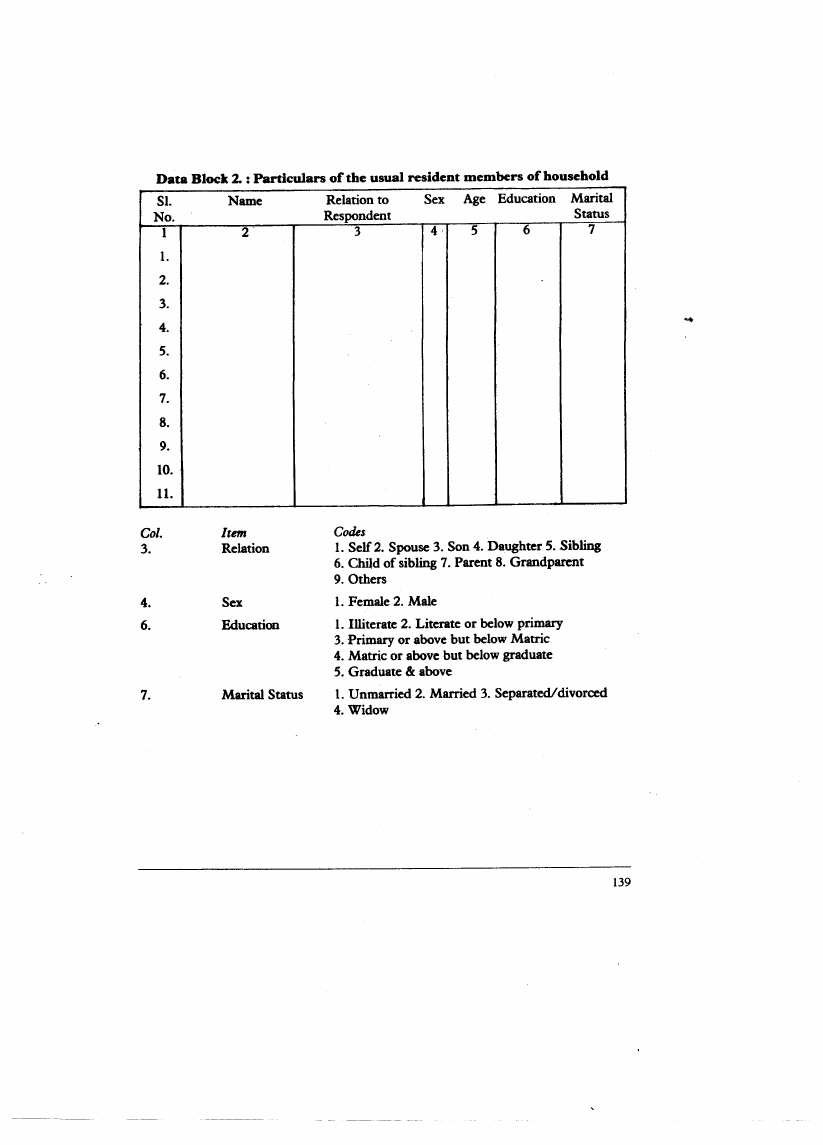
14.9 Page 139 |
▲back to top |
 |
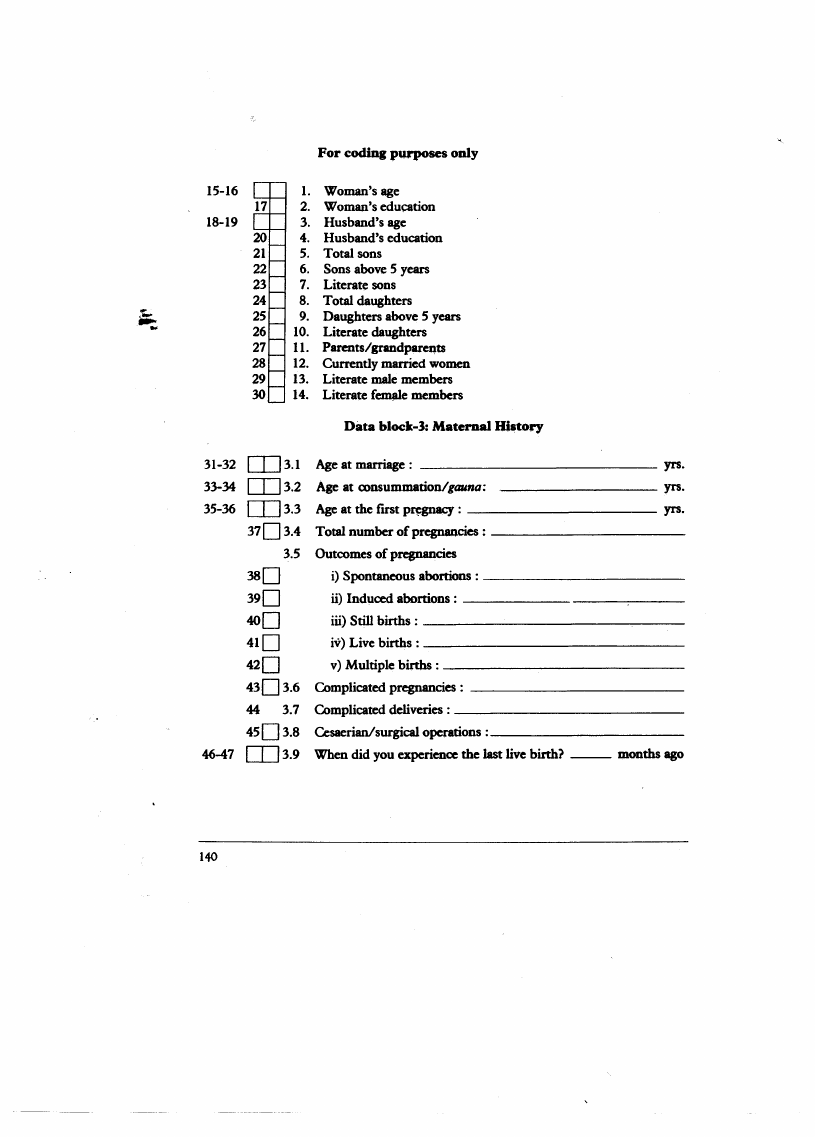
14.10 Page 140 |
▲back to top |
 |
15 Pages 141-150 |
▲back to top |
 |
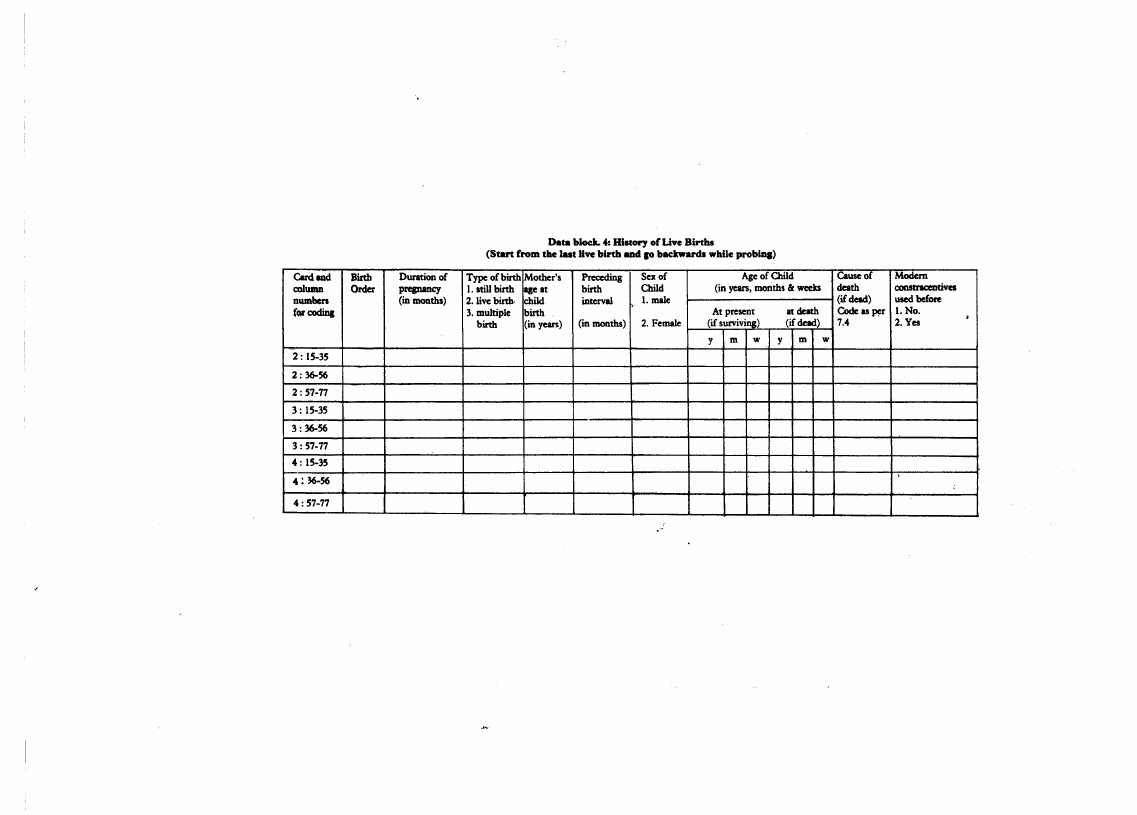
15.1 Page 141 |
▲back to top |
 |
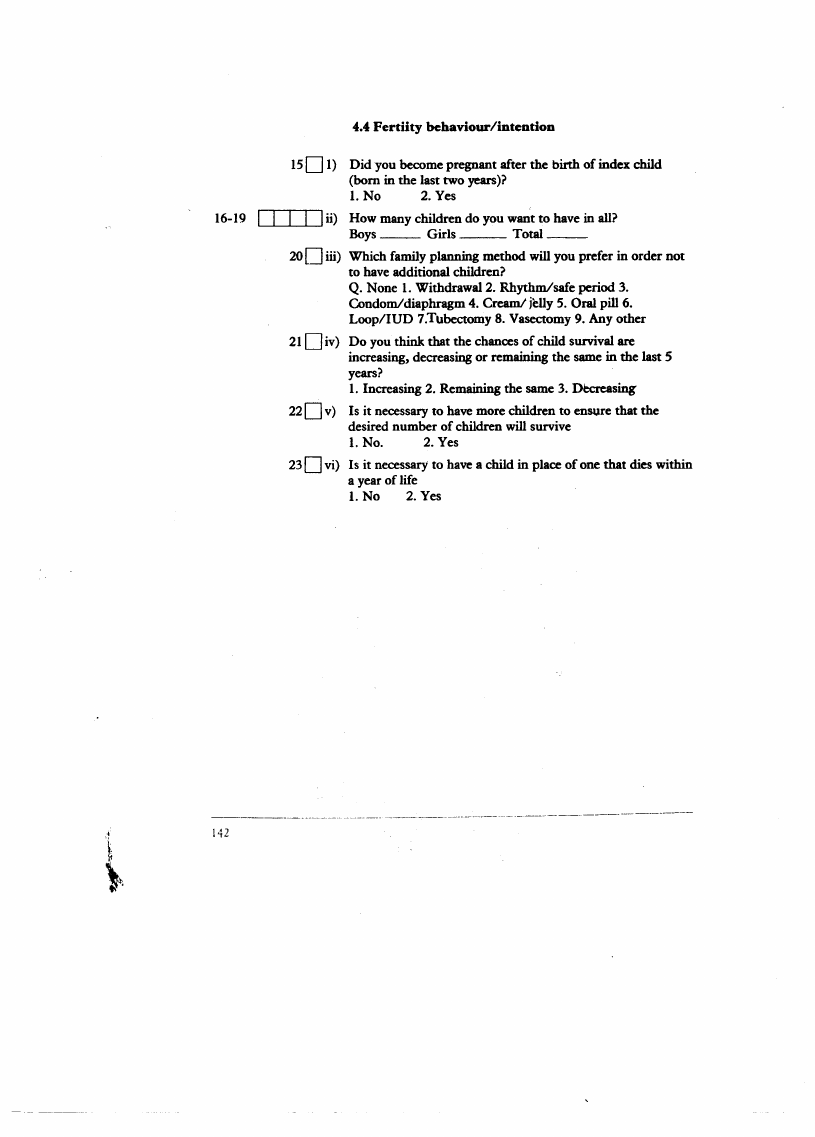
15.2 Page 142 |
▲back to top |
 |
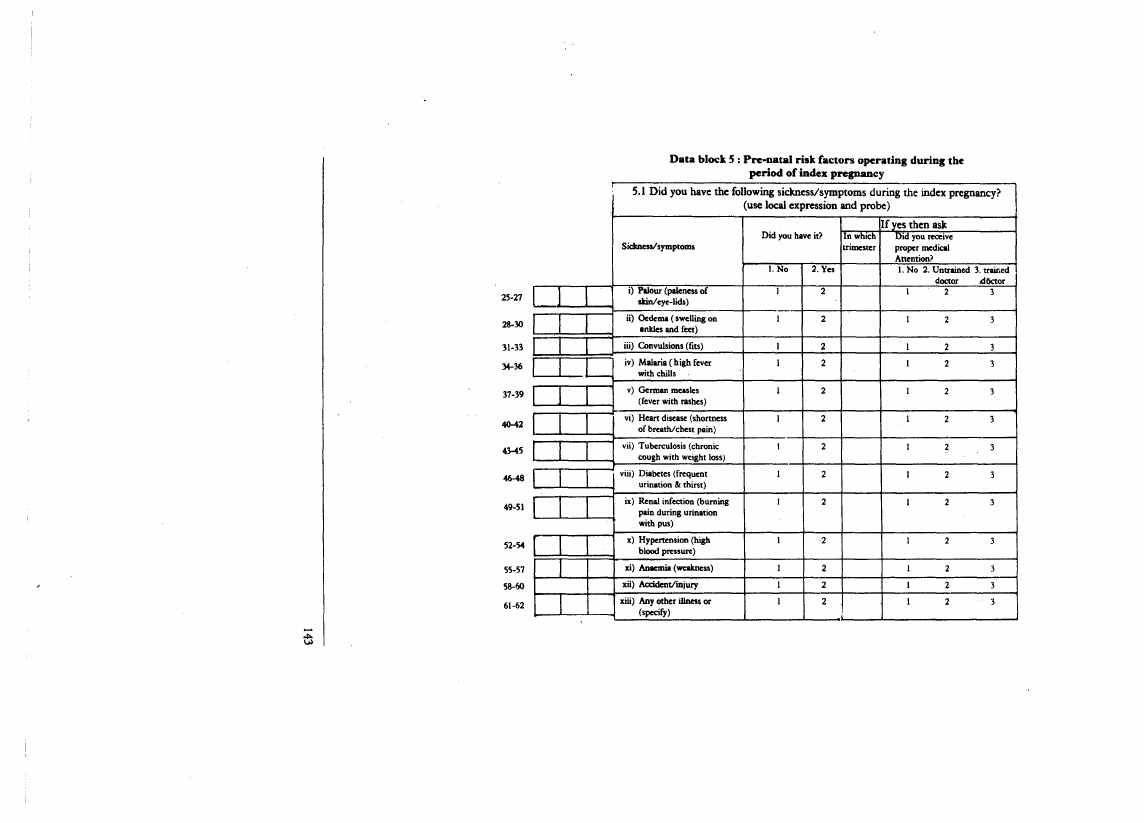
15.3 Page 143 |
▲back to top |
 |
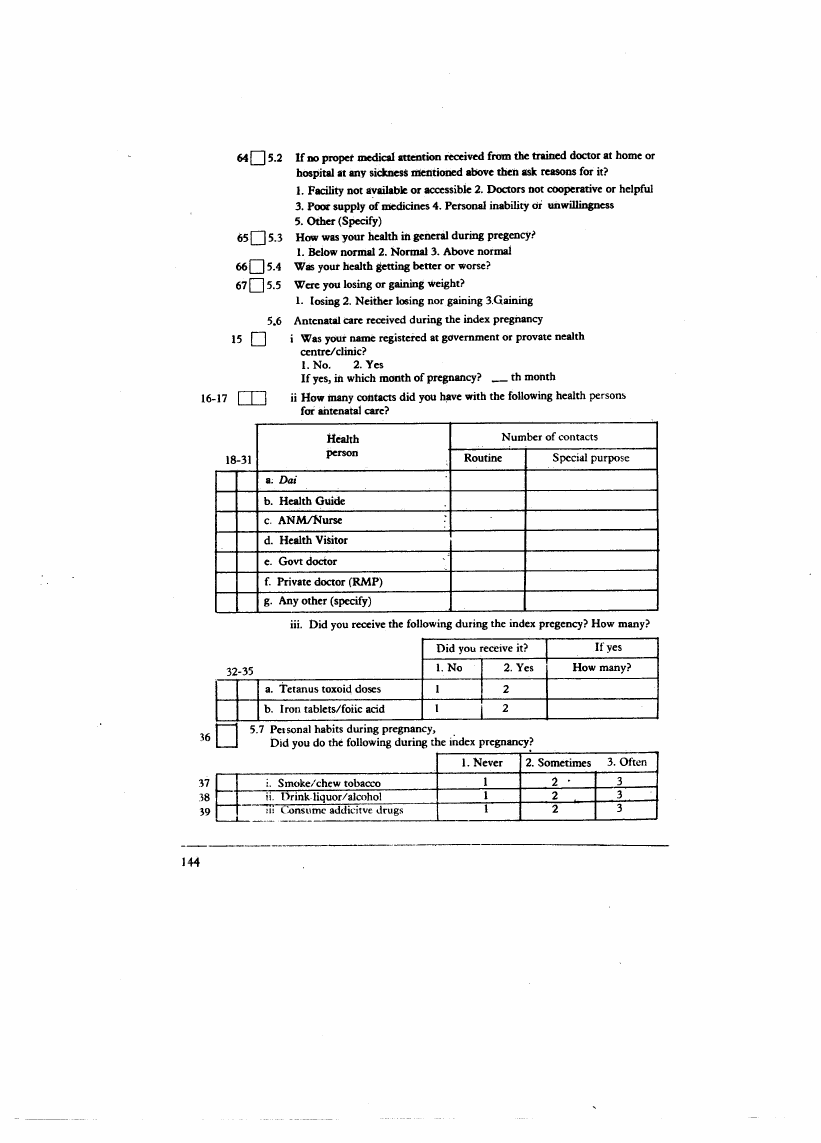
15.4 Page 144 |
▲back to top |
 |
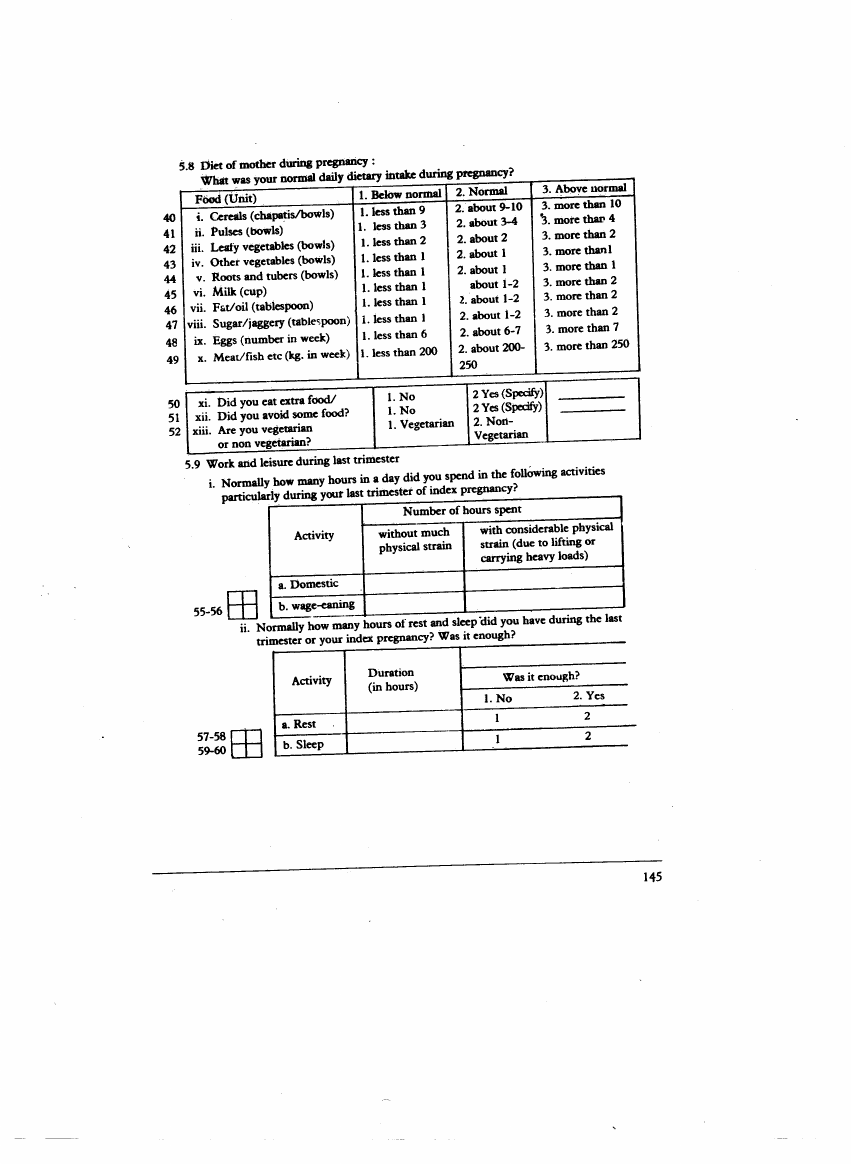
15.5 Page 145 |
▲back to top |
 |
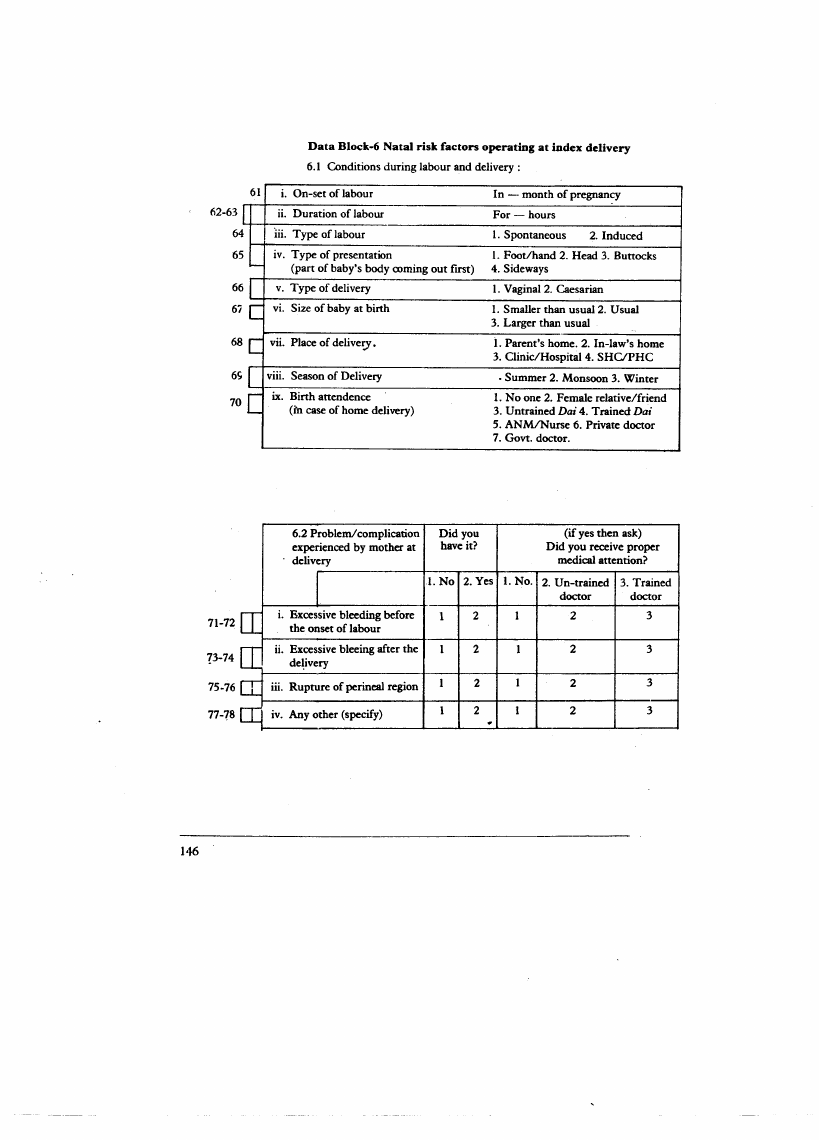
15.6 Page 146 |
▲back to top |
 |
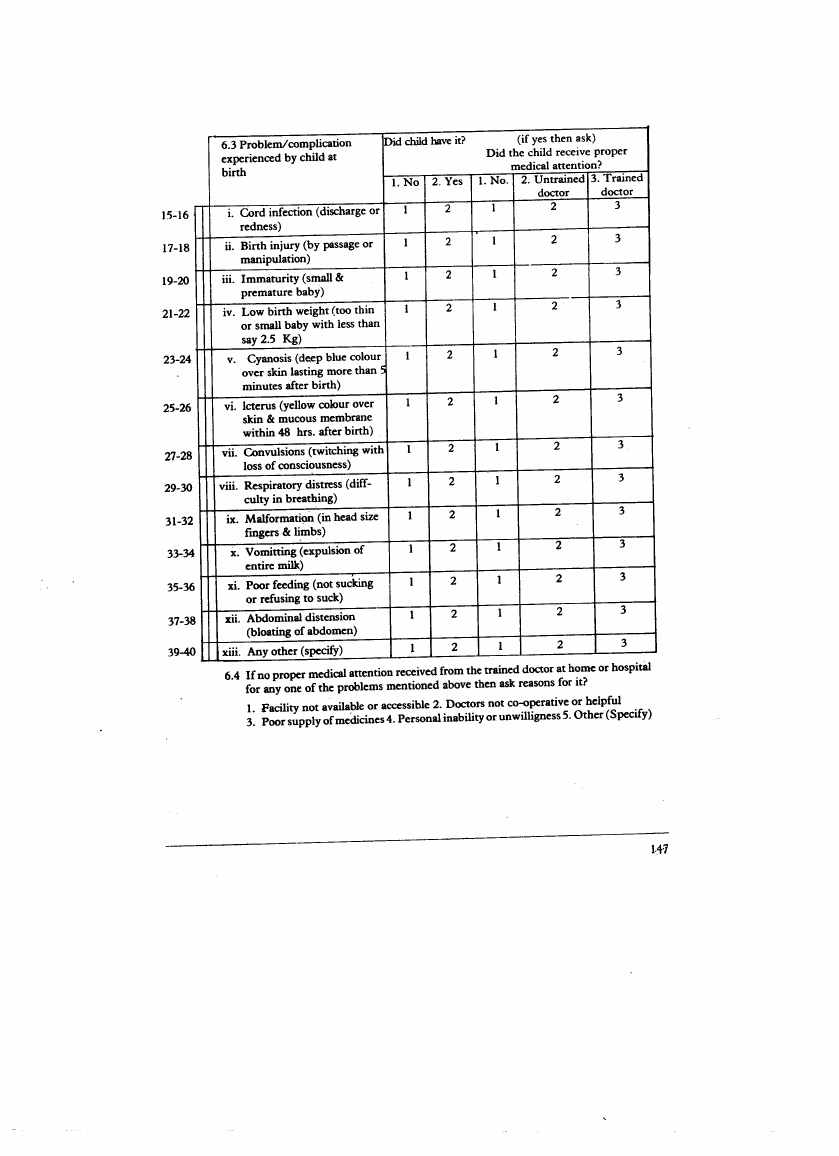
15.7 Page 147 |
▲back to top |
 |
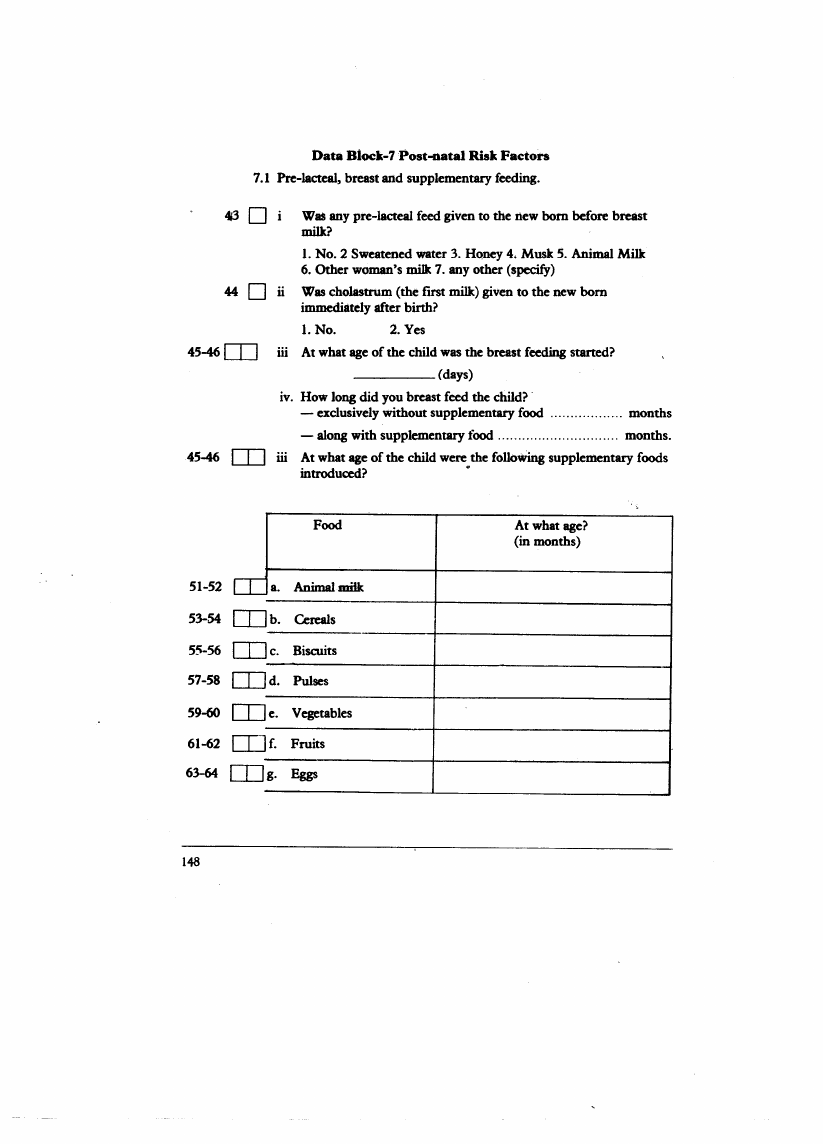
15.8 Page 148 |
▲back to top |
 |
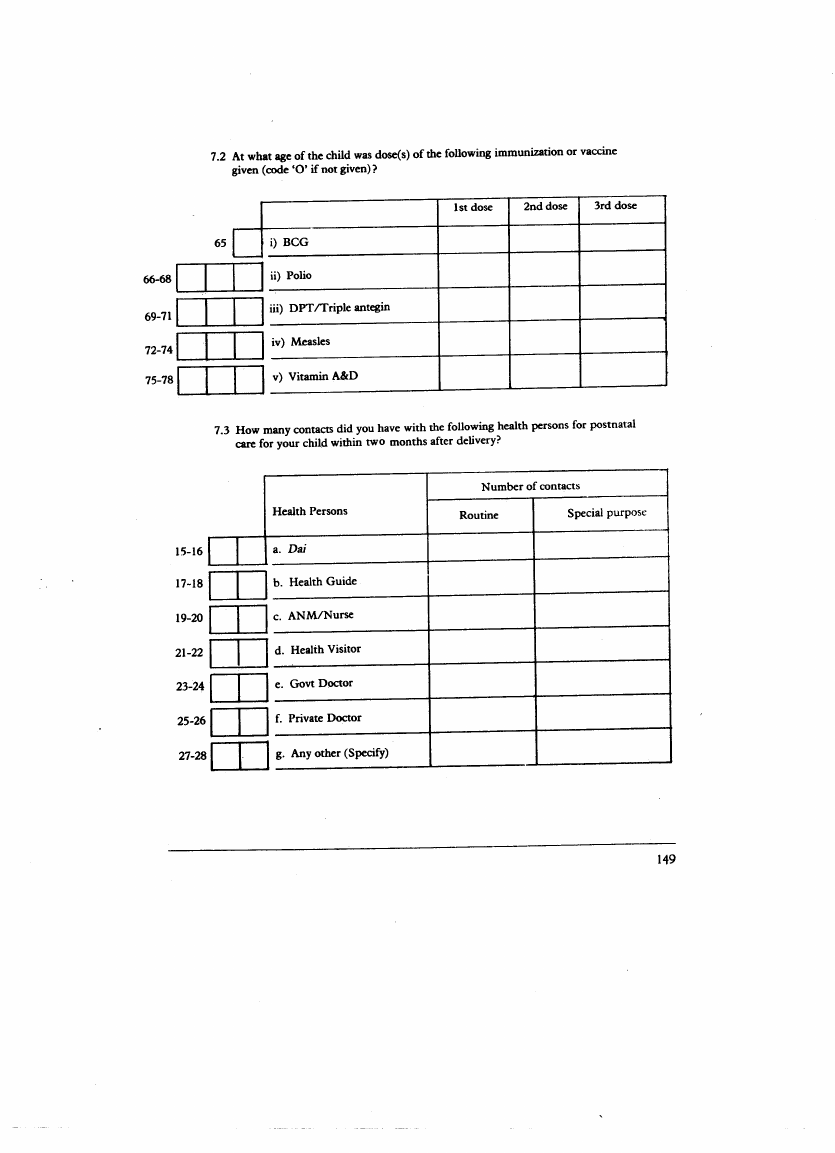
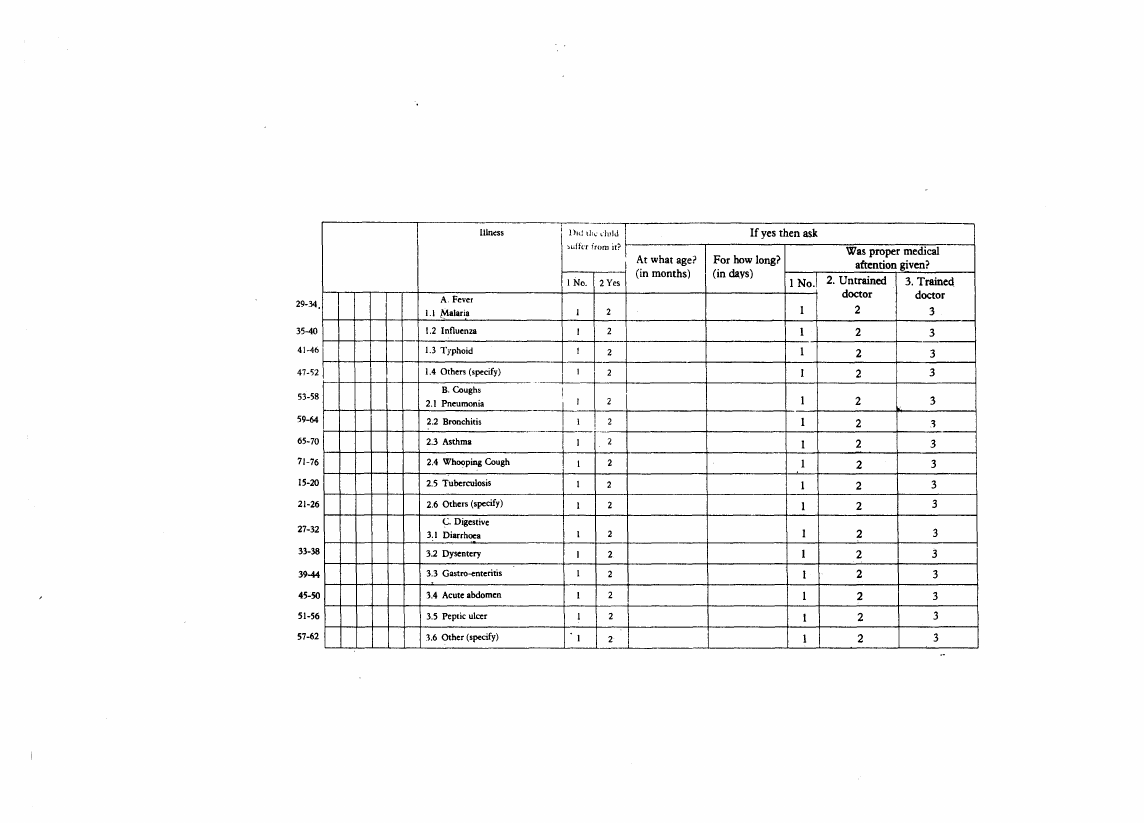
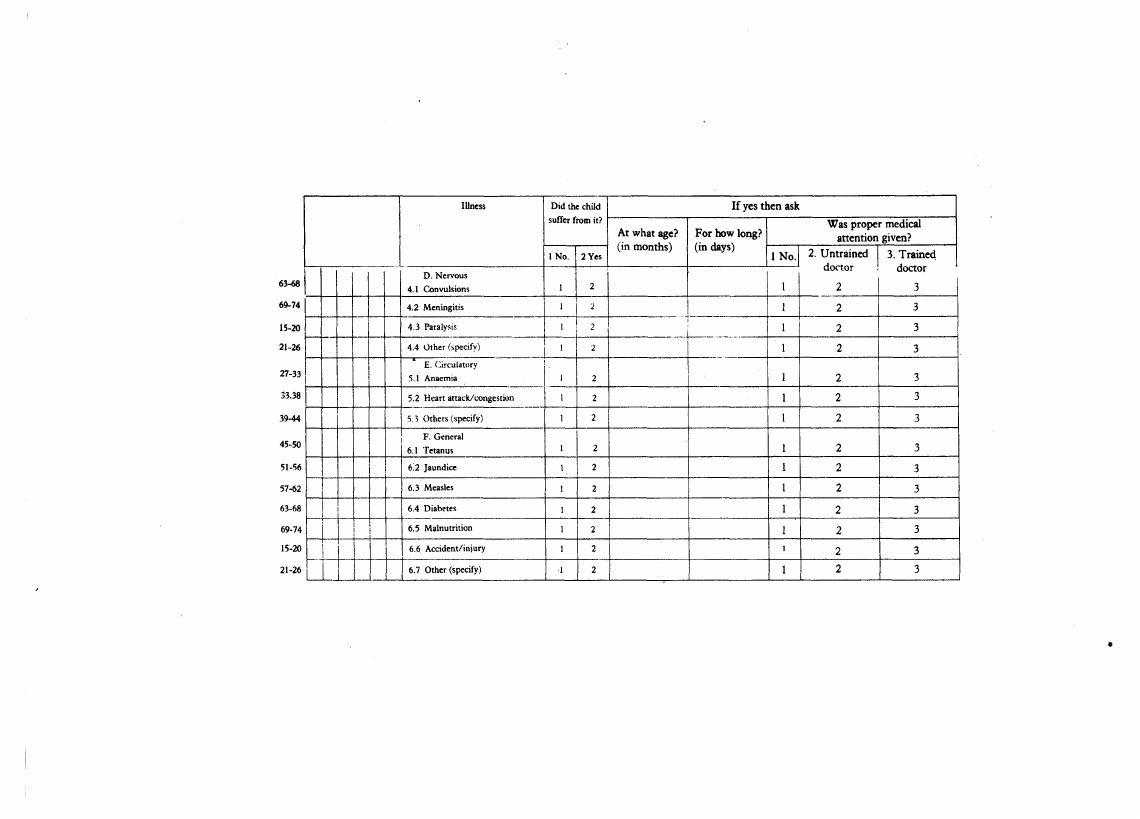
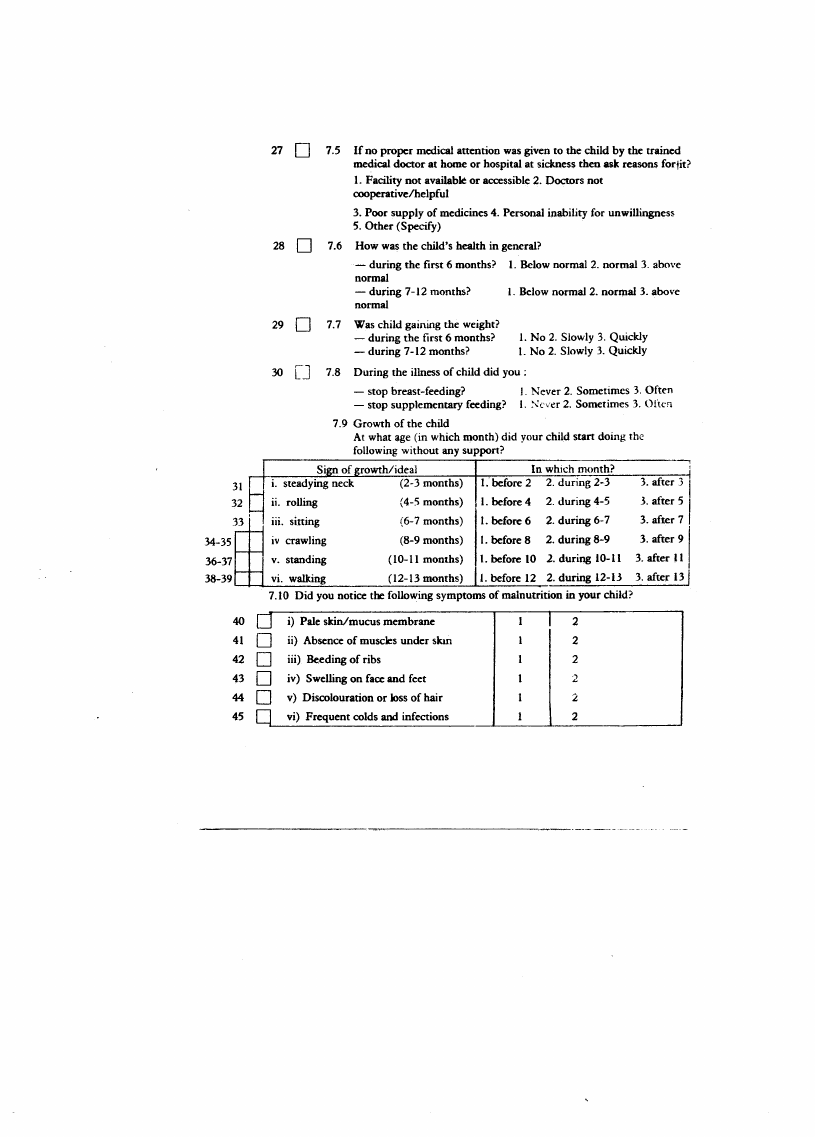
15.9 Page 149 |
▲back to top |
 |
15.10 Page 150 |
▲back to top |
 |
16 Pages 151-160 |
▲back to top |
 |
16.1 Page 151 |
▲back to top |
 |
16.2 Page 152 |
▲back to top |
 |
16.3 Page 153 |
▲back to top |
 |
16.4 Page 154 |
▲back to top |
 |
16.5 Page 155 |
▲back to top |
 |
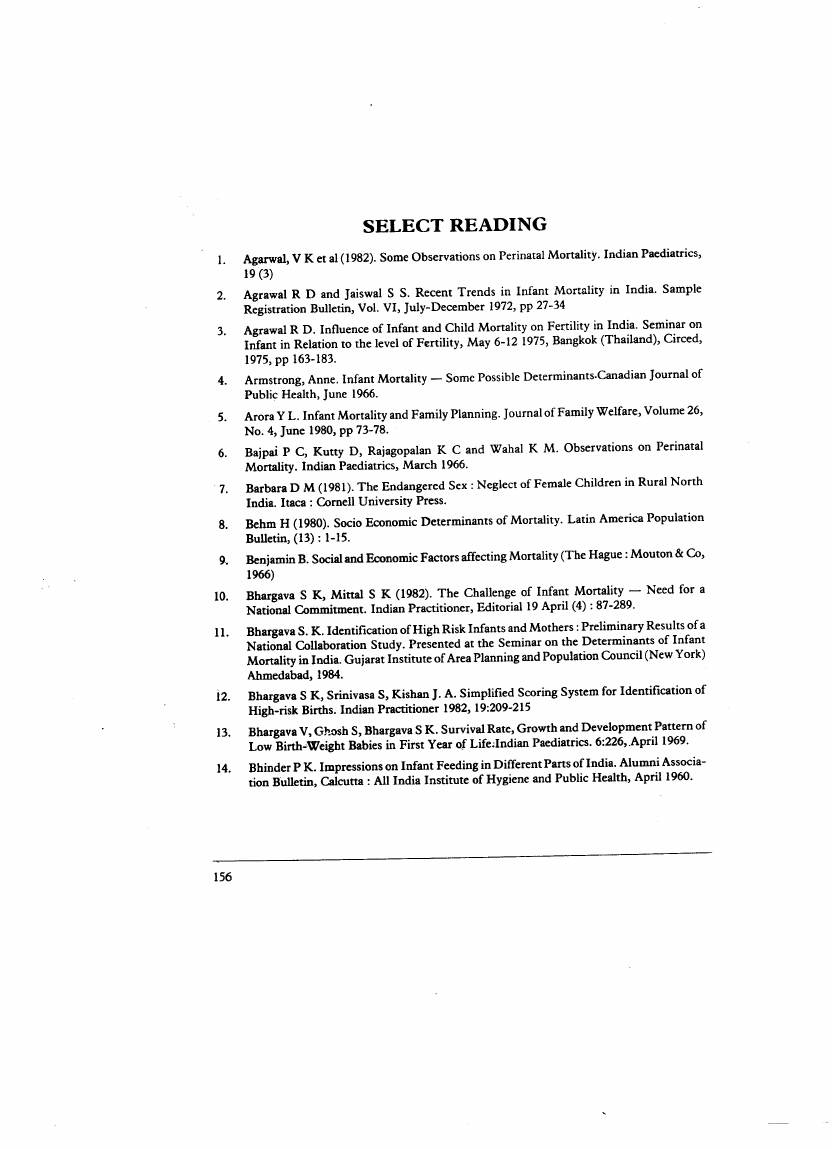
16.6 Page 156 |
▲back to top |
 |
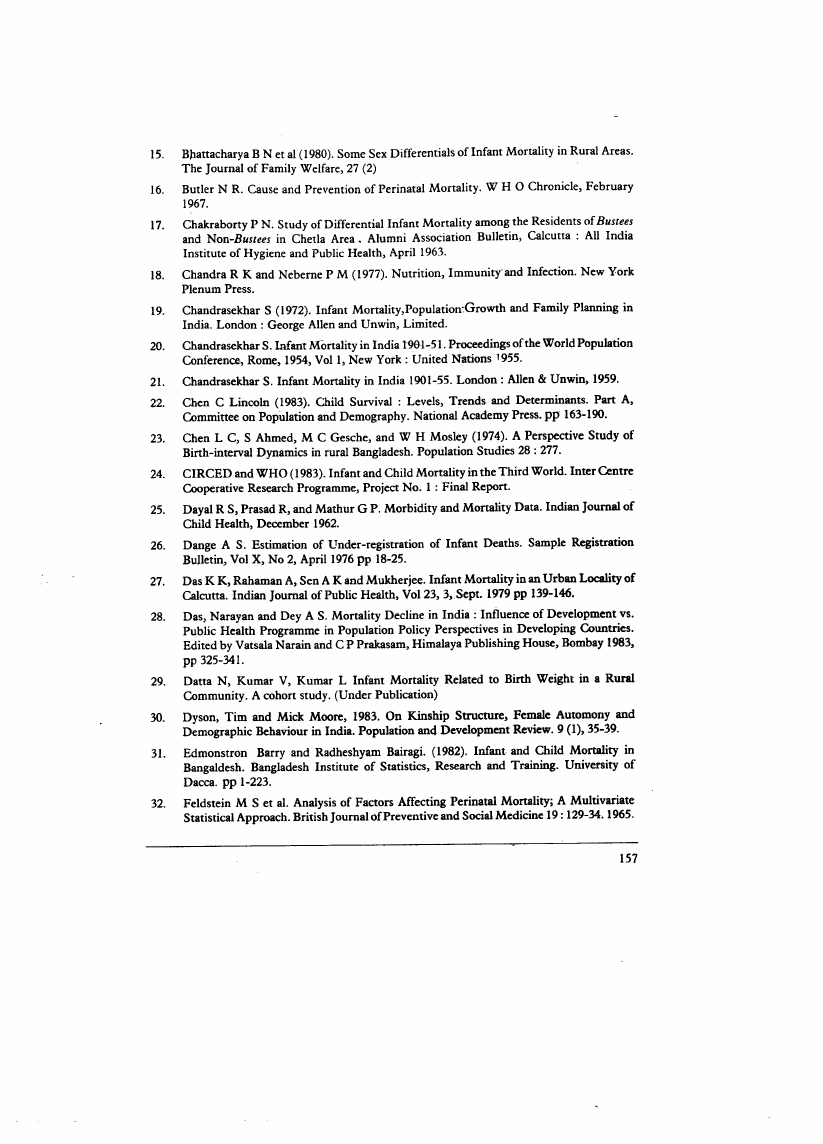
16.7 Page 157 |
▲back to top |
 |
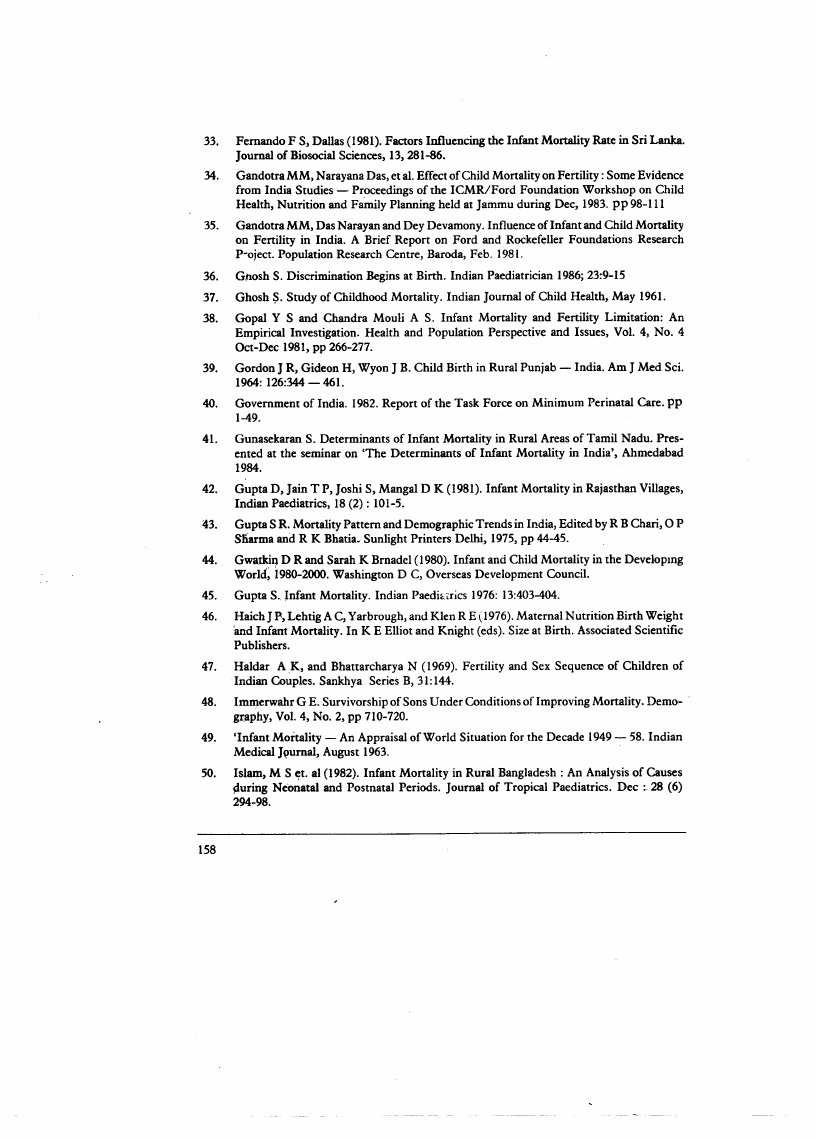
16.8 Page 158 |
▲back to top |
 |
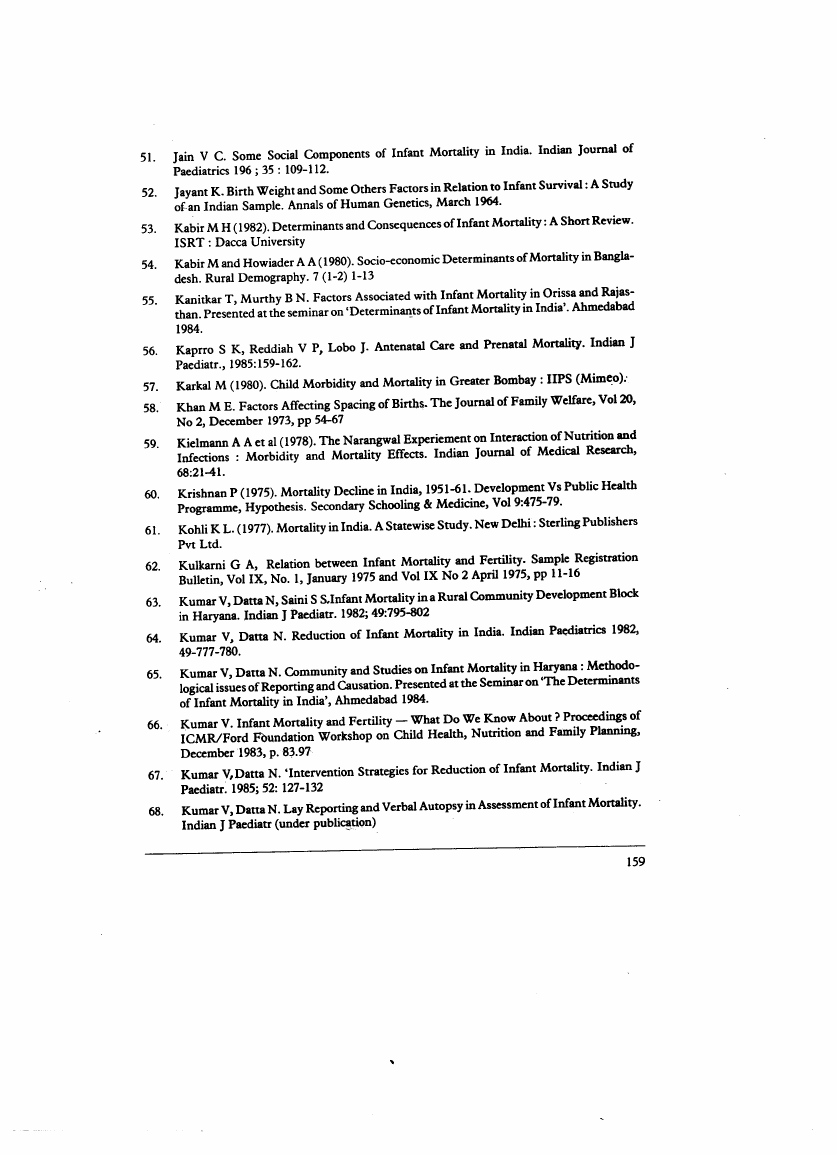
16.9 Page 159 |
▲back to top |
 |
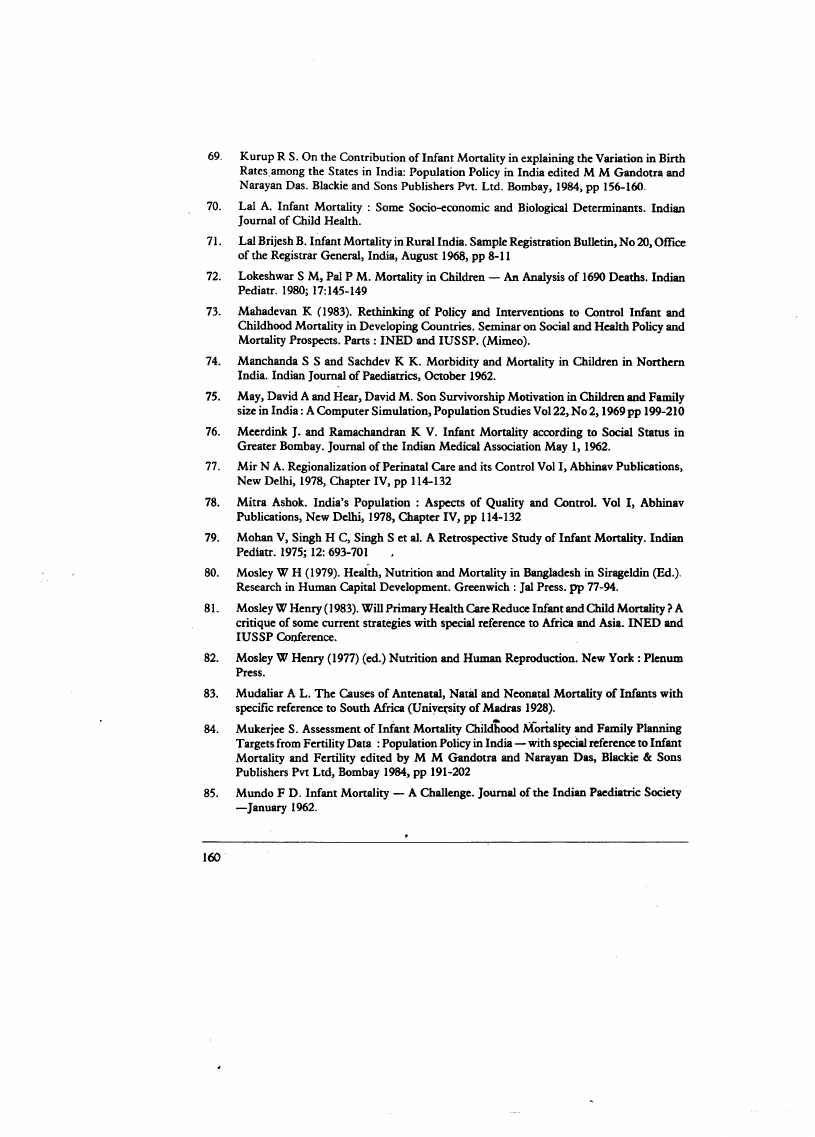
16.10 Page 160 |
▲back to top |
 |
17 Pages 161-170 |
▲back to top |
 |
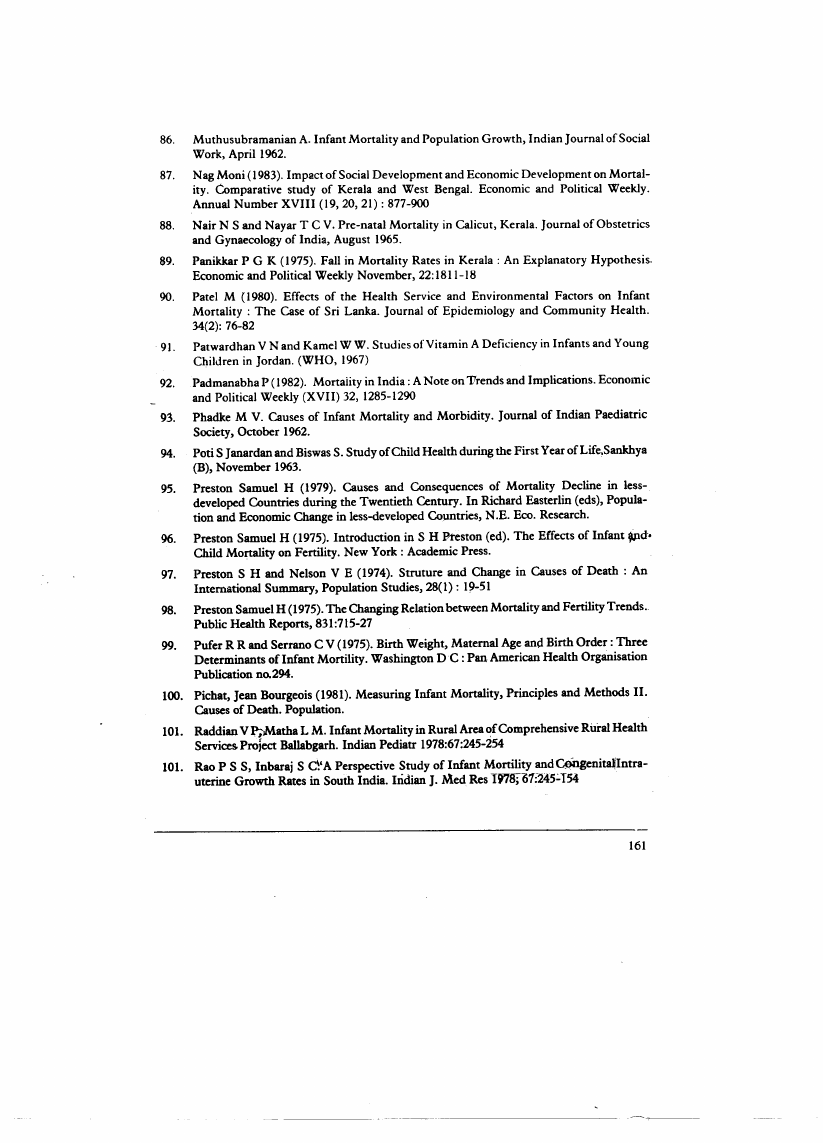
17.1 Page 161 |
▲back to top |
 |
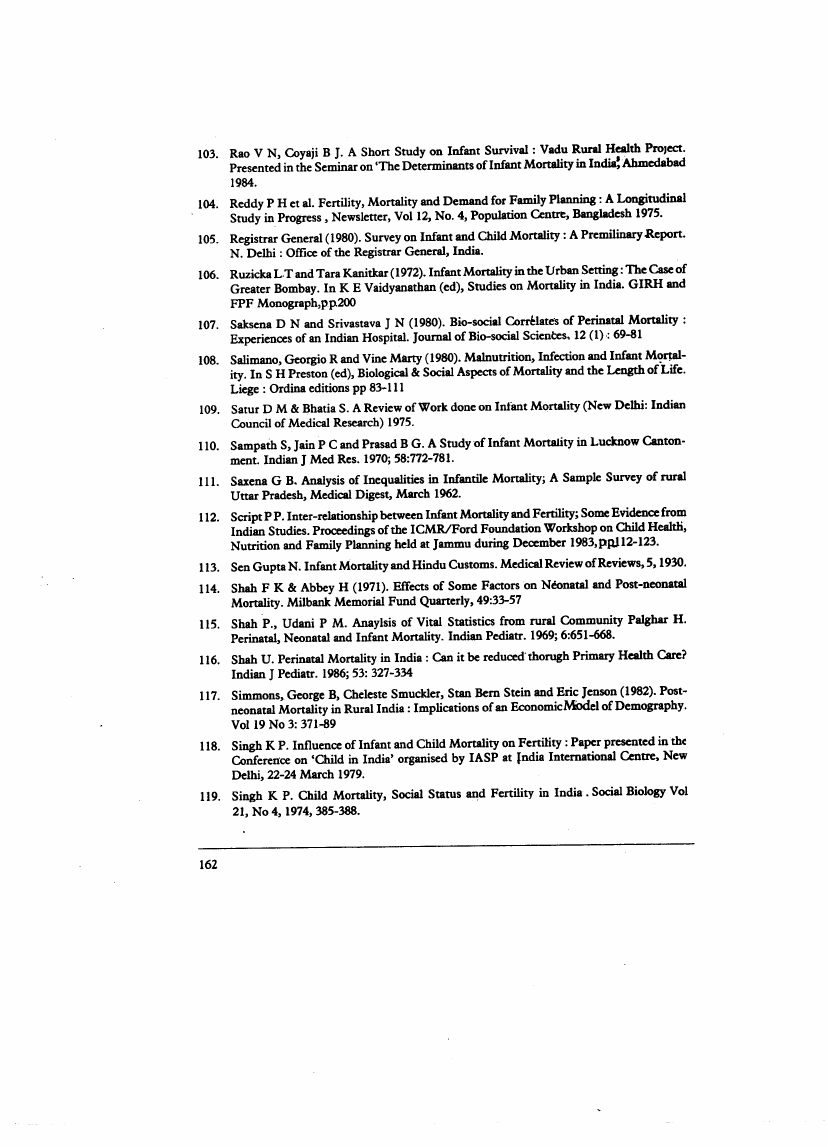
17.2 Page 162 |
▲back to top |
 |
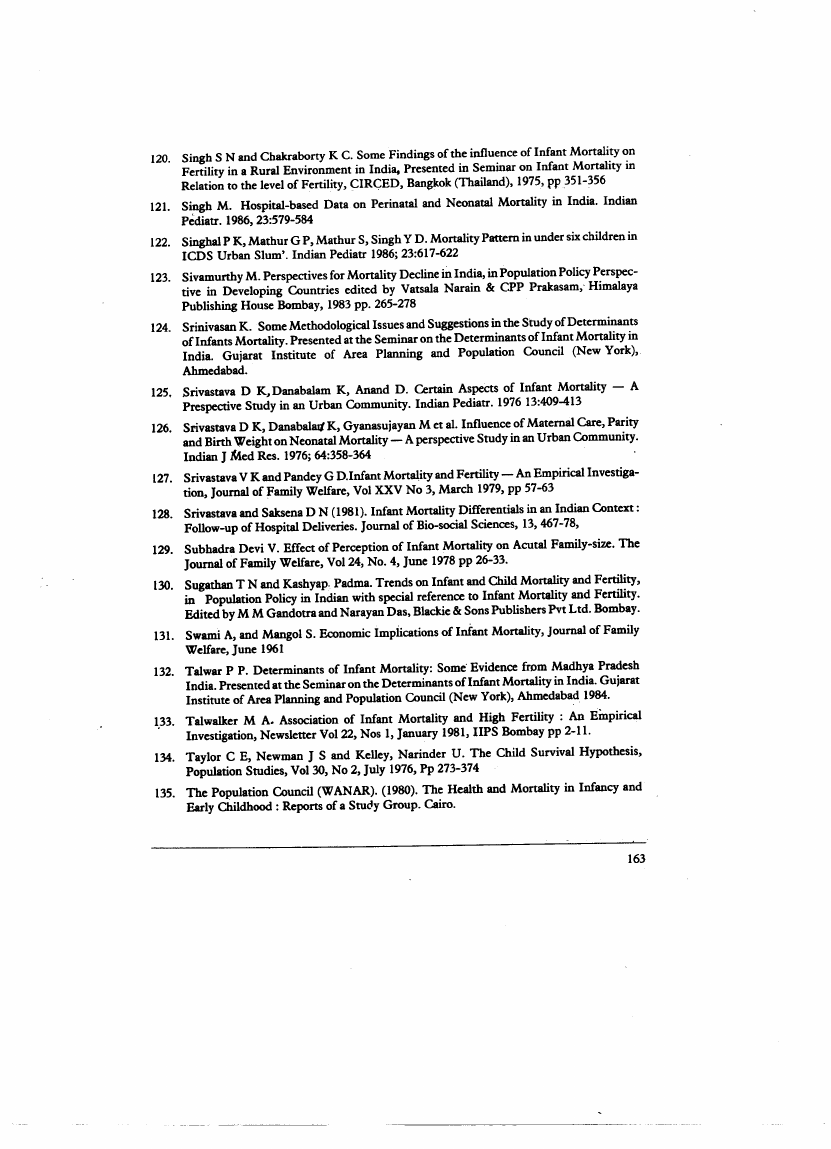
17.3 Page 163 |
▲back to top |
 |
17.4 Page 164 |
▲back to top |
 |
17.5 Page 165 |
▲back to top |
 |
17.6 Page 166 |
▲back to top |
 |
17.7 Page 167 |
▲back to top |
 |
17.8 Page 168 |
▲back to top |
 |
17.9 Page 169 |
▲back to top |