Population Foundation of India
Dissemination of Findings
The findings of the study from these centres were
shared at the national dissemination seminar. The
range of key stakeholders who participated included:
WHO India, National AIDS Research Institute,
Family Health International, Centre for Disease
Control, Indian Network for People Living With
HIV/AIDS, Plan International, Confederation of
Indian Industry, USAID, Christian Medical
Association of India, National Institute of Medical
Statistics, and other organizations and experts
involved in the issues of care and support to PLHAs.
The centres that had taken part in this study also
participated.
The dissemination seminar critiqued mentioned that
globally, human rights/legal needs constituted a
separate category in them and the model presented in
this dissemination lacked the human rights aspect,
which is important in the context of HIV/AIDS. It
was also felt that economic support is an important
component of care and support and should be
included in the model. In fact the comprehensive
approach to care and support should be within a
continuum in order to meet the varied material,
psycho-social, and medical needs of PLHA and those
affected.
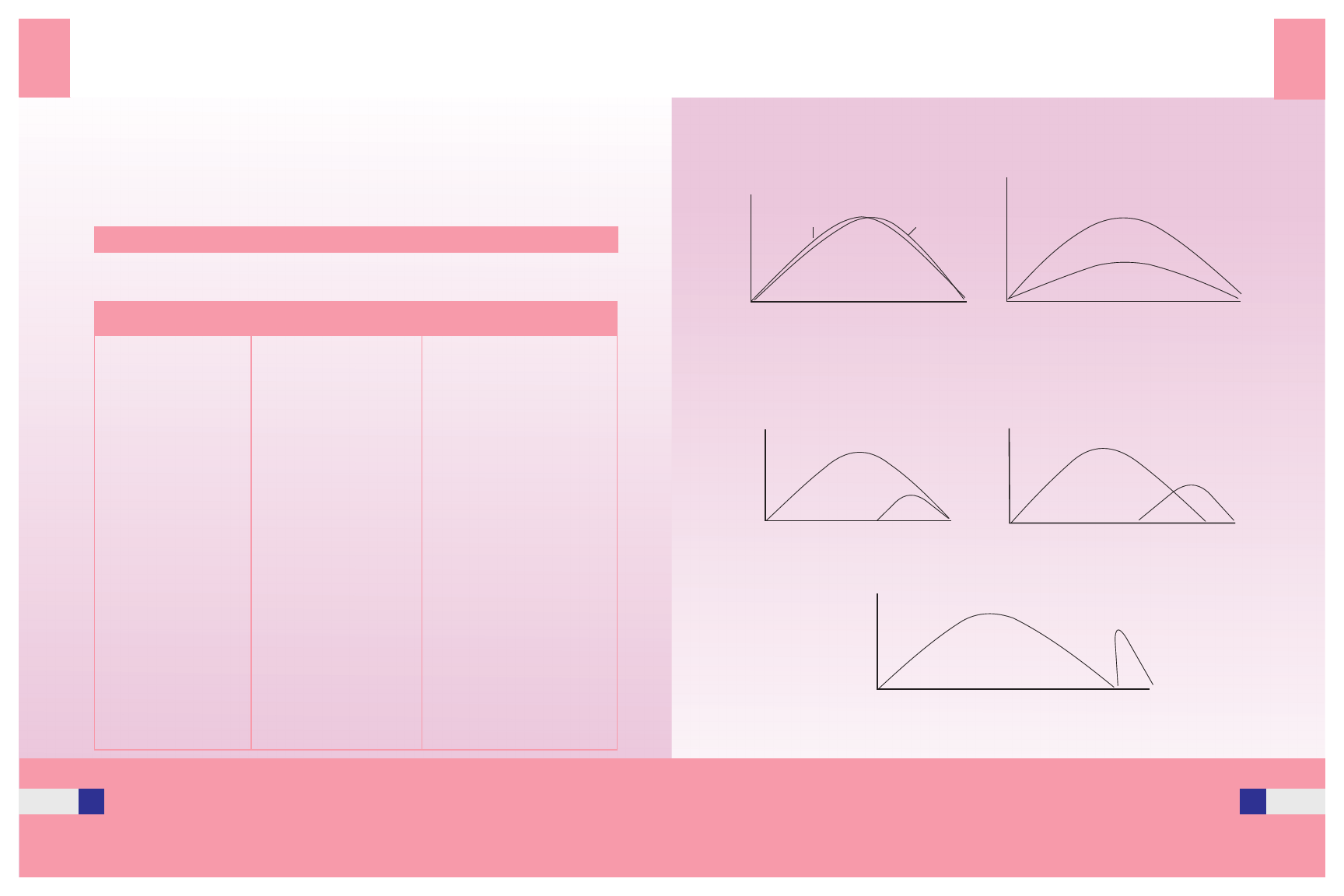
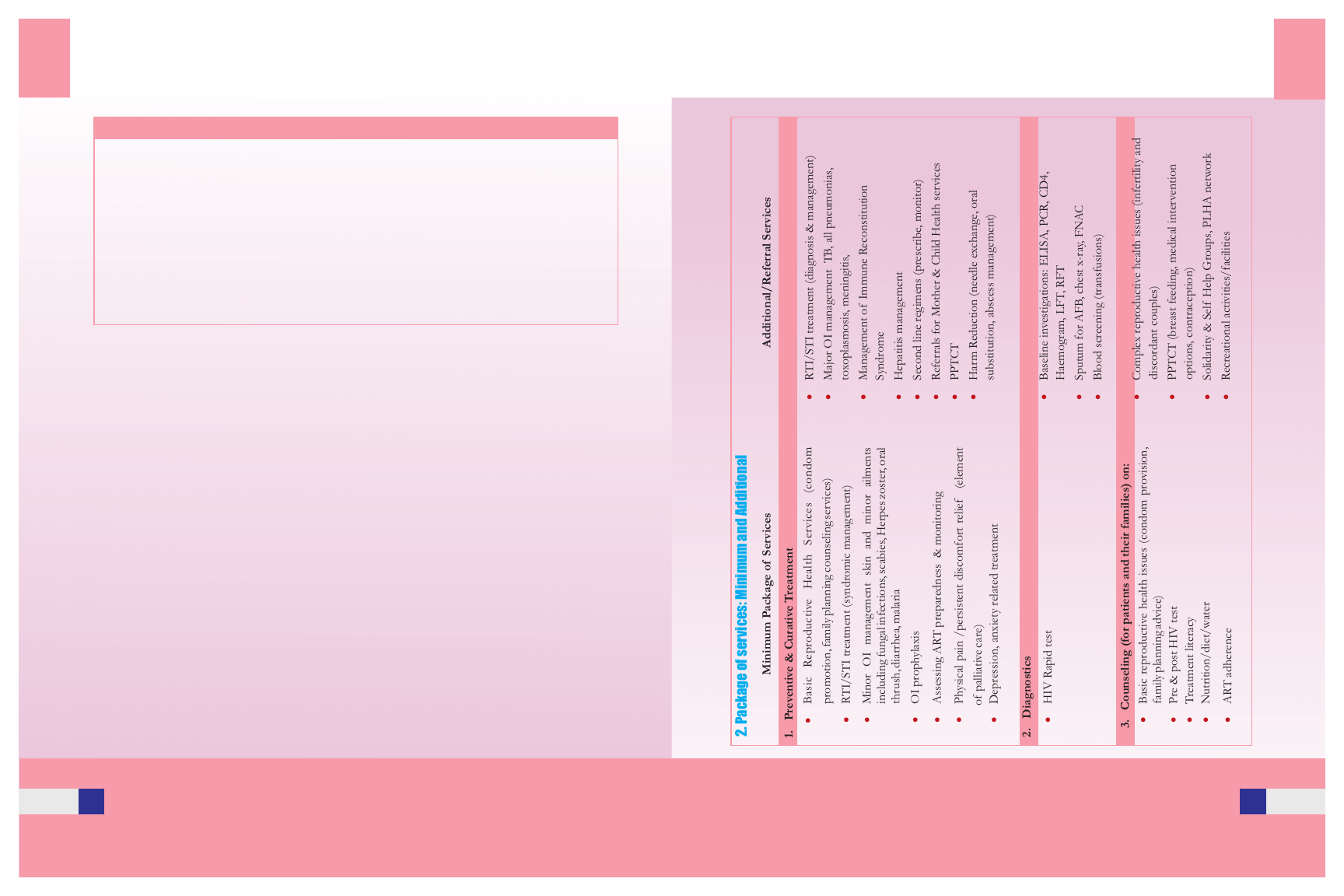
In terms of the actual services listed under the above
categories (see Table 1), participants offered various
suggestions and comments. While some felt that
getting the CD 4 count done at a care centre would be
next to impossible and that should come under
“referrals”, others suggested that this decision be
based on the requirements of each state and its social
and legal situation. It was unanimously agreed that
STI related services including diagnosis needed to be
a separately categorized and that psycho-social
services should be included at every stage, not just at
the beginning. It was also suggested that referral
services be included right from beginning.
The components of a comprehensive service
package were deliberated upon. The NACO
guidelines were also discussed.
According to NACO in NACP II, the concept of
comprehensive HIV/AIDS care across the
continuum of care builds on HIV/AIDS care
services in a team spirit and includes the following:
· Voluntary counseling and testing
· Clinical management
· Nursing care
· Pre and post test counseling
· Care and home and in the community
· Formation of community support groups
· Eliminating stigma
· Social support or referral to appropriate
social welfare services
· Partnership building between various
providers
Source: http://www.nacoonline.org/guidelines/guideline_6.pdf
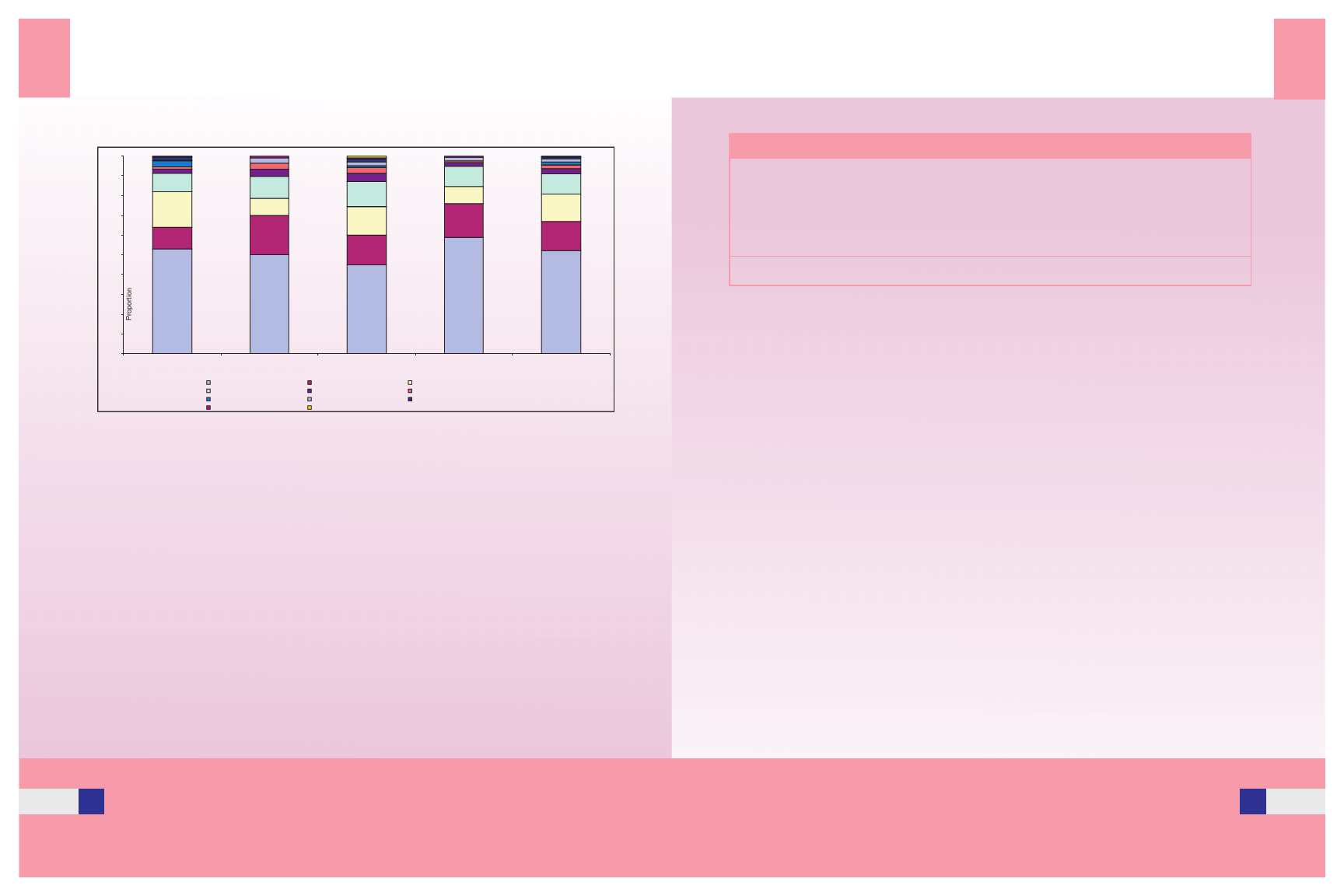
The dissemination seminar discussed various key
issues that are presented here:
Defining Comprehensive Care
Comprehensive Care meets the diverse needs of
people living with and affected by HIV, builds trust
and creates a receptive audience among patients,
10
Guidelines for Care and Support Services
families and other community members and
enhances prevention efforts. It paves the way for
community acceptance of people living with HIV
and decreases stigmatization. Comprehensive care
was defined here as that which made economic,
psycho-social, physical, political and legal support
available to PLHAs and those affected by the
epidemic. The components of a system of
comprehensive care included psycho-social support;
life-skills training; community, family and partner
support, access to nutrition and a hygienic
environment, treatment of OIs; access to affordable
ART, palliative care and legal support. The provision
of care should also offer opportunities to make
prevention interventions more accessible and
available, and encourage those who receive it to
practice safer behaviour. Particularly essential to this
HIV care are counseling policies and practices that
ensure a better quality of life for people.
different facilities needed to be considered. DOTS
centres and whether care homes should have this
facility was another issue touched up on.
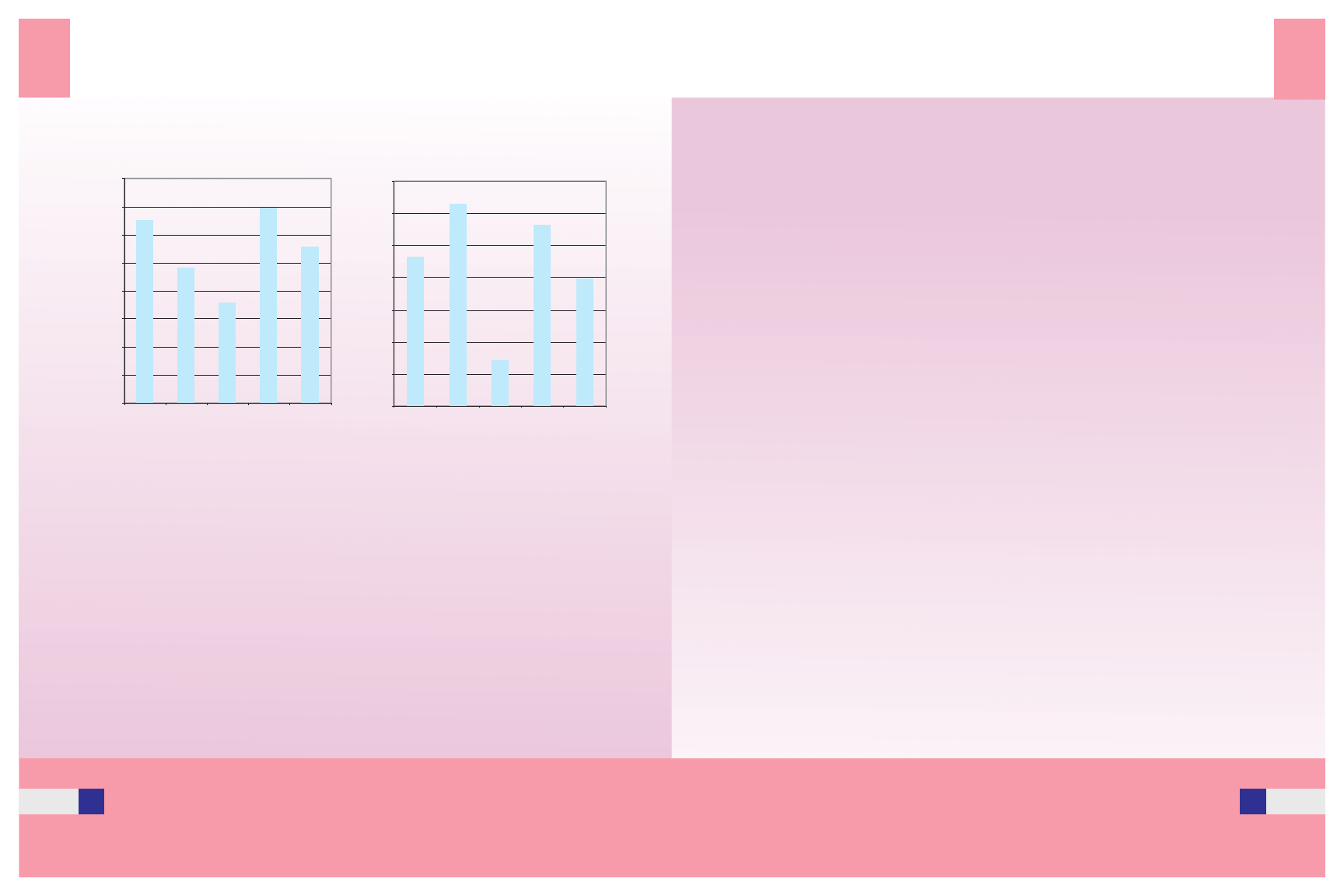
Networks antd Referrals
Networking and developing referral linkages are
practical approaches for addressing the different
needs that arise in the domain of care and support.
Specific practical partnerships can be developed and
referral plans to ensure a continuum of care and
support for PLHA. It is often inappropriate for care
centers to provide some services that are a key
component of care and support. Other kinds of
inputs are needed, for example if income generation
activities are being supported, they should be coupled
with an organization with experience in micro-credit.
A recommendation of NACP II has been to link
VCTCs with at risk communities and available care
and support centers in the area.
Diagnostics
Another concern expressed was the need to qualify
“diagnostics” for the purpose of clarity. Some felt
that the provision of a rapid HIV test was essential
and part of the minimum package at a care centre.
This was based on the fact that people were admitted
into a care facility only after they had a positive test
report, and testing done via a referral system caused a
delay, which affected the patient's health adversely. A
concern expressed by a participant was that while a
one-stop shop was an ideal situation, could centres
really scale up to that level? Aside from the kits
needed, the operational factors involved in including
Antiretroviral Therapy
Antiretroviral drugs are one component of a
comprehensive HIV/AIDS program that also
includes prevention and other care and support
facilities. A significant achievement of NACPII has
been the introduction and subsequent scale-up of
ART through the public health system. A
recommendation has been to strengthen the existing
mechanisms to improve coverage and compliance of
the ART regimen, which includes utilizing and
strengthening existing care centers. The immediate
task then is to integrate ART into the continuum of
care, treatment and prevention and situating it within
the existing health system.
11