 |
Issue Briefs - NRHM Decentralized System |
 |
1 Page 1 |
▲back to top |
Table 4: Details of NRHM Components
Component
Details
Accredited Social Health
Activists (ASHA)
One female voluntary worker in every village per population of 1000*; coordinates and promotes various health and
sanitation programmes in the village; helps prepare and implement the Village Health Plan; receives performance based
compensation
Sub-Centres (SCs)
Provide an annual United Fund and maintenance fund of Rs 10,000 each; provide medicines; create additional sub-centres;
improve existing facilities
Primary Health Centres
(PHCs)
Provide a constant supply of drugs and medical equipment; make 24hr medical services available in half of the PHCs; allocate
additional resources for disease prevention programmes; increase staff to two doctors; add a 24hr referral service in all PHCs
Community Health Centres Rogi Kalyan Samitis (stakeholder committees) for hospital management; devise standards for hospital services and costs;
(CHCs)
develop and comply with a Citizen’s Charter
District Health Plans
Create district health plans using goals for health, nutrition, water, and sanitation to guide planning, implementation, and
monitoring of NRHM; merge other district and state level health and family welfare programmes under this district health plan
Sanitation and Hygiene
Promote sanitation and hygiene activities through the Village Health & Sanitation Committee; merge existing sanitation
and hygiene programmes under NRHM
Disease Control
Programmes
Create initiatives for controlling the spread of diseases; launch disease surveillance system at the village level; provide a
district mobile medical unit for outreach programmes; merge National Disease Control programmes for malaria, TB, kala
azar, filarial, blindness & iodine deficiency under NRHM
Public-Private Partnerships Increase regulation of private-sector healthcare services; create guidelines for public-private partnerships
Health Financing
Mechanisms
Form a task group to study financing healthcare; create standards for all medical services; constitute a National Expert
Group to review and advise on financing healthcare
Health/Medical Education Make health education supportive of rural health issues; create new medical and para-medical facilities on a needs basis
*Note: ASHA workers are only for high-focus states and tribal areas in other states, but some states have applied this in other areas.4
Sources: Ministry of Health & Family Welfare, National Rural Health Mission ‘Mission Document’; NRHM Broad Framework for Preparation of District Health Action Plan; NRHM Framework for
Implementation 2005-2012.
Budget Allocations
The NRHM budget will incorporate all health related
schemes and expenditures under the Eleventh Plan. The
funds under NRHM are distributed to the respective
Health Societies (permanent bodies providing guidance
and management) at the state and the district levels.
Allocation of funds is done on the basis of population,
disease burden, health indicators, state of public health
infrastructure, etc.3
Endnotes
1. Ministry of Health & Family Welfare, NRHM. ‘Rural
Healthcare System in India’. March 2007. See http://mohfw.nic.
in/Bulletin%20on%20RHS%20-%20March,%202007%20-
% 2 0 P D F % 2 0 Ve r s i o n / R u r a l % 2 0 H e a l t h % 2 0 C a r e % 2 0 S y s t e m
%20in%20India.pdf.
2. Ministry of Health & Family Welfare, NRHM. ‘National Rural
Health Mission: Mission Document’. See http://mohfw.nic.in/NRHM/
Documents/NRHM%20Mission %20Document.pdf.
3. Ministry of Health & Family Welfare, NRHM. ‘Framework for
Implementation 2005-2012’. See http://mohfw.nic.in/NRHM/
Documents/NRHM%20-%20Framework%20for%20Implementation.
pdf.
4. Ministry of Health & Family Welfare, NRHM. ‘Common Review
Mission Report’. See http://mohfw.nic.in/NRHM/Documents/CRM_
report_full_report_version.pdf.
5. Ministry of Health & Family Welfare, NRHM. ‘Major Stakeholders
& Their Roles’. See http://mohfw.nic.in/NRHM/stakeholders.
htm#sg.
DISCLAIMER: This document is being furnished to you for your information. The opinions expressed herein are entirely those of the author(s). PFI & PRS
makes every effort to use reliable and comprehensive information, but PRS does not represent that the contents of the report are accurate or complete. PRS
is an independent, not-for-profit group. This document has been prepared without regard to the objectives or opinions of those who may receive it.
Population Foundation of India
B-28, Qutab Institutional Area, New Delhi-110016
Tel.:+91-11-43894100, Fax: +91-11-43894199,
E-mail: popfound@sify.com, Website: www.popfound.org
National Rural Health Mission–
Decentralized System
ISSUE BRIEF
Context
• Rural healthcare is provided at three levels: the sub-centre, the primary health centre,
and the community health centre. In total, there are 171,687 rural healthcare centres as
of March 2007.
• The Ministry of Health and Family Welfare (MHFW) launched the National Rural
Health Mission (NRHM) in April 2005 to provide comprehensive and affordable
healthcare in rural areas. The NRHM will continue to operate until 2012.
• The scheme covers all states but gives special consideration and assistance to 18 ‘high
focus’ states with weak public healthcare systems and facilities.
• High focus states have an Accredited Social Health Activist (ASHA) in villages with a
population of at least 1000 as well as state and district level project support.
• One of the main aims of the Mission is to bridge the gap between rural and urban
healthcare, improve hospital care and management, and create a decentralized system
that enables a consolidation of health schemes and effective use of resources.
• Key components of the NRHM include creating accredited social health activists,
strengthening existing health centres, creating district health plans, guiding sanitation
and hygiene projects, and strengthening disease control programmes.
• Under NRHM, healthcare is managed at the local level. The plan uses the Panchayati Raj
Institutions (PRI) to undertake and implement the programmes under this scheme.
• The village, gram panchayat, cluster, block, and district level health committees are
responsible for creating local specific health plans and health related activities.
Prepared by
PRS Legislative Research, Centre for Policy Research, Dharma Marg, Chanakyapuri, New Delhi – 110021
 |
2 Page 2 |
▲back to top |
Context
The Ministry of Health and Family Welfare (MHFW)
launched the National Rural Health Mission in 2005
to increase access to quality and affordable healthcare
in rural areas. The aim of NRHM is to “bridge the
gap in rural healthcare through creation of a cadre of
Accredited Social Health Activists (ASHA) and improve
hospital care, decentralization of programme to district
level to improve intra and inter-sectoral convergence
and effective utilization of resources.”1
Goals for the National Rural Health Mission (2005-2012)
• Reduce the Infant and Maternal Mortality Rate
• Provide universal access to public health services
• Prevent and control spread of diseases
• Provide access to primary healthcare
• Promote population, gender and demographic balance
• Revitalize local health traditions
• Encourage healthy lifestyles
Source: Ministry of Health & Family Welfare, NRHM, ‘Mission Document’.
The scheme covers all states but focuses on 18 states with
weak public health indicators or health infrastructure.2
These states will have an Accredited Social Health
Activist in villages with a population of 1000 as well as
state and district level project support.3
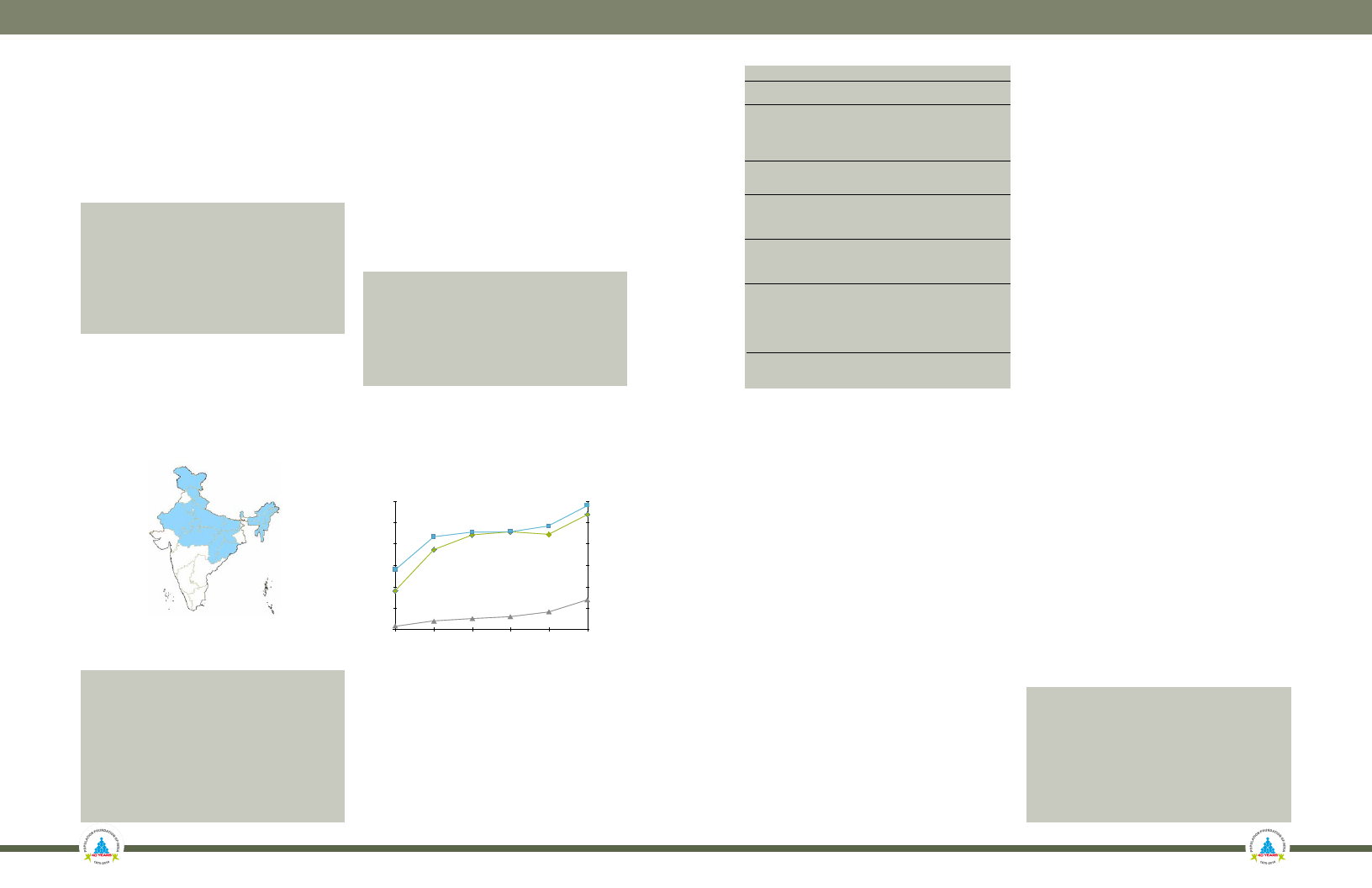
Figure 1 shows the 18 high focus states.
Figure 1: High Focus States
Decentralized Rural Healthcare
Currently, rural healthcare services are provided at three
levels: the sub-centre (SC), the primary health centre
(PHC), and the community health centre (CHC). The SC
provides basic health services to the villagers and refers
more serious cases to the PHC. The PHC encompasses
about six sub-centres and focuses on preventative and
curative health practices. The CHC usually covers the
area of four PHCs and provides specialized care and
consultations.1
Table 2 below provides an overview of the existing rural
healthcare centres.
Table 2: Rural Healthcare Centres
(As of March 2007)
Centre Population Villages Staff Existing
Covered
Covered
Centres
SC
3000-5000
4
2-3 145,272
PHC 20,000- 30,000
29
14
22,370
CHC 80,000-120,000 158
25
4,045
Total
171,687
Sources: Ministry of Health & Family Welfare, NRHM, ‘Rural Healthcare System in India’; PRS.
Figure 2 show the growth of healthcare centres
beginning with the Sixth Plan and include
projections for additional centres under the
NRHM.
Figure 2: Trends in Rural Health Centres
NRHM Target Outcomes
Table 1: Targets for Some Key Health Indicators
Indicators
Target Rate
Infant Mortality
30/1000 live births
Maternal Mortality
100/100,000 live births
Total Fertility Rate
2.1
Malaria Mortality Reduction 50% by 2010, additional 10% by 2012
Dengue Mortality Reduction 50% by 2010, elimination by 2012
Kala Azar Mortality Reduction 100% by 2010, sustain until 2012
Filaria/Microfilaria Reduction 70% by 2010, 80% by 2012,
& elimination by 2015
Tuberculosis DOTS series 85% cure rate through 2012
Leprosy Prevalence
1/100,000 prevalence rate
Sources: Ministry of Health & Family Welfare, NRHM ‘Framework for Implementation’.
30,000
25,000
Sub Centres (Right Hand Scale)
180,000
150,000
20,000
15,000
Primary Health Centres
120,000
60,000
10,000
5,000
Community Health Centres
60,000
30,000
0
0
VI Plan VII Plan VIII Plan XI Plan X Plan NRHM
Coverage
Sources: Ministry of Health & Family Welfare, NRHM, ‘Rural Healthcare
System in India’; PRS.
NRHM Structure
The committees, plans and programmes under the
NRHM are executed at various institutional levels.
One of the key aims of the NRHM is to bring the
management of healthcare to the local level. The
plan uses the Panchayati Raj Institutions (PRI) to
undertake and implement the programmes under this
scheme.
Table 3: NRHM Committees
Level Committees
Village • Village Health & Sanitation Committee
• Village Health Plan & Register
Gram • Sub-Centre Health Level Committee
Panchayat • Gram Panchayat Level Health Plans
• Cluster Primary Healthcare PRI Committee
• Cluster Level Health Plan
• Rogi Kalyan Samiti
Block/ • Block Level Monitoring and Planning Committee
CHC
• Block Health Plan
• Rogi Kalyan Samiti
Zila
• District Health Mission
Parishad • District Health Action Plan
(District • Mobile Medical Unit
Level) • Programme Management Units
State • State Health Mission
• State Health Plan
• Integration of Departments of Health & Family Welfare
• Programme Management Units
National • National Mission Steering Group
• Empowered Programme Committee
• Standing Mentoring Group
• Task Groups for Selected Tasks
• Integration of Health & Family Welfare Departments
• National Expert Group
Sources: Ministry of Health & Family Welfare, NRHM Health Mission ‘Mission Document’;
NRHM Broad Framework for Preparation of District Health Action Plan; NRHM Framework for
Implementation 2005-2012.
Village Level
The village health and sanitation samiti includes members
of the panchayat, ANM/MPW, anganwadi workers,
teachers, ASHA, community health volunteers, etc. The
committee prepares the village health plan, the village
register, and the household survey. The combination of
all village health plans form the gram panchayat, cluster
block and finally district level plans.5
Gram Panchayat
The sub-centre health level committee reports to the gram
panchayat that oversees and supports the village level
household survey and health plan. The gram panchayat
level health plan is a consolidation of plans from multiple
villages.3
Cluster
The PHC committee consults with the panchayat and
the community to create a cluster level plan. The cluster
oversees sub-centre work and any health activities at the
gram panchayat level.3 The Rogi Kalyan Samiti has two
main functions: (a) use public participation to increase
accountability, and (b) increase quality and maintenance
of health facilities.4
Block Level
The block level group includes the adhyaksha (head) of
the block panchayat samiti, the block medical officer, the
block development officer, NGO representative, and the
head of the CHC Rogi Kalyan Samiti. The block level
group manages the household surveys and organizes
public health events to help with the plan preparation.3
Zila Parishad/District
The district level team includes the zila parishad adhyaksha,
the district medical officer, and the district magistrate.
The district mission supervises and assists in creating a
draft district health plan, which is “the key strategy for
integrated action under NRHM.”3 The district level
group also organises public events to help with the plan
preparation.3 The district plans are reviewed by the state
health mission, which also monitors district compliance to
the citizen’s charter (a document for citizens health rights).
Finally, the district mission is responsible for submitting
the annual work plan, budgets, and perspective plan to
the state level mission.3
State Level
Each state government is responsible for ensuring the
proper functioning of NRHM. The state organizes
stakeholder workshops, prepares a state action plan,
develops a district strategy for vulnerable populations, and
oversees the health programmes run by the Panchayati Raj
Institutions. It also provides guidelines for the formation
of health committees and the selection and training of
the ASHA workers.5
National Level
There are several national level committees constituted to
monitor and oversee the implementation of the NRHM.
The committees include: (a) a national mission steering
group headed by the Union Minister for Health & Family
Welfare; (b) empowered programme committee chaired
by the secretary of HFW; and (c) standing mentoring
group to oversee the ASHA component. In addition, the
mission can constitute issue specific tasks groups.
Components of the NRHM Scheme
In addition to the ASHA scheme, NRHM proposes
to (a) strengthen existing village sub-centres, primary
healthcare centres, and community healthcare centres;
(b) form district health plans; (c) guide sanitation
and hygiene projects under NRHM; (d) strengthen
disease control programmes; (e) foster public-private
partnerships in healthcare; (f) implement new finance
mechanisms; and (g) revise health education.5
Janani Suraksha Yojana (JSY)
• Centrally funded scheme that uses cash incentives to promote
institutional delivery among BPL women
• Goal is to reduce maternal and infant mortality
• Applies to BPL pregnant women above 19 years for up to two live
births (up to three live births in 10 states)
• For each delivery, the mother gets up to Rs 1400 and the ASHA up to
Rs 600
Source: Ministry of Health & Family Welfare.





