Repositioning Family Planning A review of evidence of effective interventions_ English
 |
Repositioning Family Planning A review of evidence of effective interventions_ English |
 |
1 Pages 1-10 |
▲back to top |
 |
1.1 Page 1 |
▲back to top |

 |
1.2 Page 2 |
▲back to top |

 |
1.3 Page 3 |
▲back to top |

 |
1.4 Page 4 |
▲back to top |
 |
1.5 Page 5 |
▲back to top |

 |
1.6 Page 6 |
▲back to top |
 |
1.7 Page 7 |
▲back to top |
 |
1.8 Page 8 |
▲back to top |
 |
1.9 Page 9 |
▲back to top |

 |
1.10 Page 10 |
▲back to top |

 |
2 Pages 11-20 |
▲back to top |
 |
2.1 Page 11 |
▲back to top |

 |
2.2 Page 12 |
▲back to top |
 |
2.3 Page 13 |
▲back to top |
 |
2.4 Page 14 |
▲back to top |

 |
2.5 Page 15 |
▲back to top |
 |
2.6 Page 16 |
▲back to top |

 |
2.7 Page 17 |
▲back to top |
 |
2.8 Page 18 |
▲back to top |
 |
2.9 Page 19 |
▲back to top |

 |
2.10 Page 20 |
▲back to top |

 |
3 Pages 21-30 |
▲back to top |
 |
3.1 Page 21 |
▲back to top |

 |
3.2 Page 22 |
▲back to top |
 |
3.3 Page 23 |
▲back to top |

 |
3.4 Page 24 |
▲back to top |
 |
3.5 Page 25 |
▲back to top |

 |
3.6 Page 26 |
▲back to top |

 |
3.7 Page 27 |
▲back to top |

 |
3.8 Page 28 |
▲back to top |
 |
3.9 Page 29 |
▲back to top |
 |
3.10 Page 30 |
▲back to top |

 |
4 Pages 31-40 |
▲back to top |
 |
4.1 Page 31 |
▲back to top |
 |
4.2 Page 32 |
▲back to top |
 |
4.3 Page 33 |
▲back to top |

 |
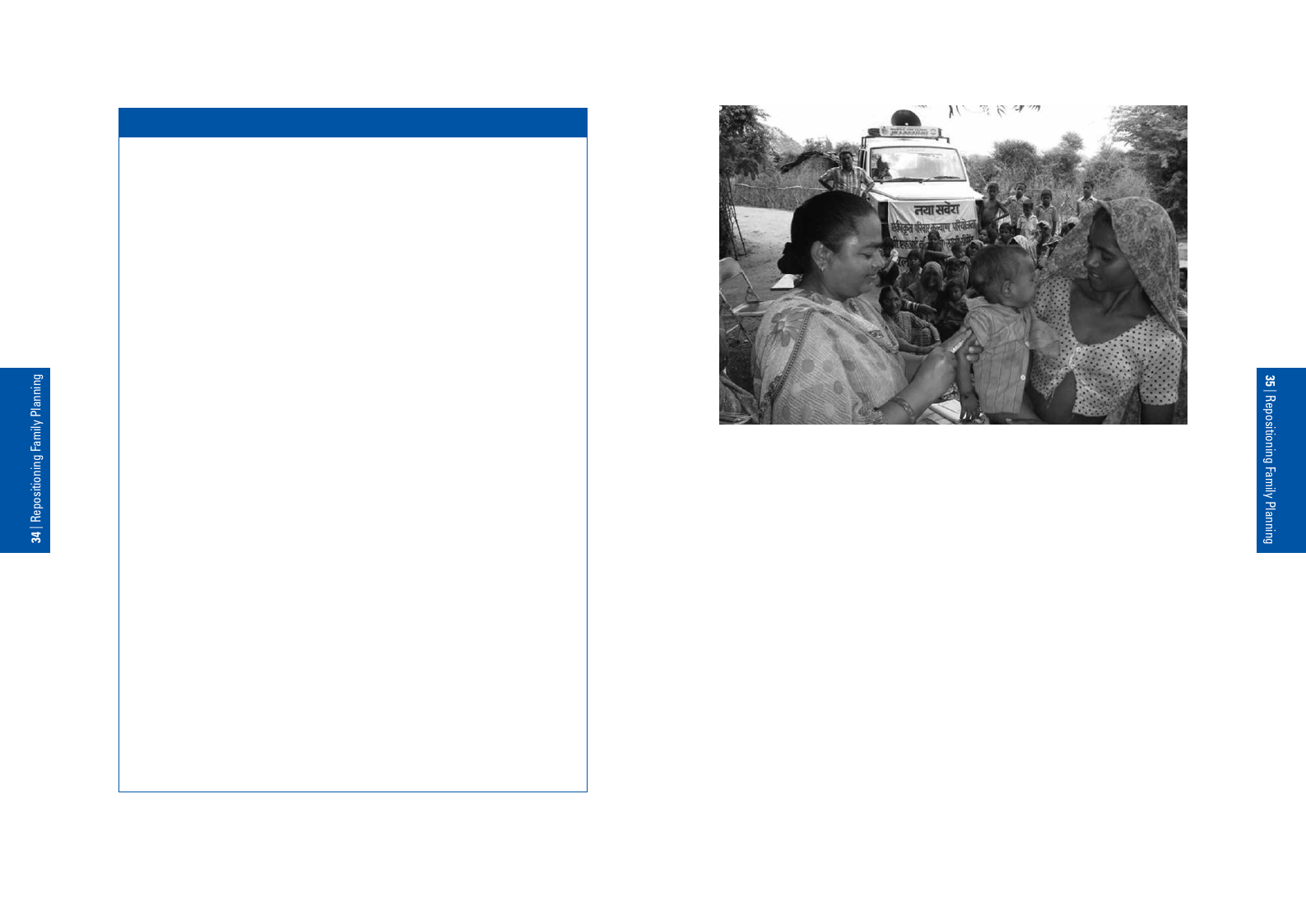
4.4 Page 34 |
▲back to top |

 |
4.5 Page 35 |
▲back to top |

 |
4.6 Page 36 |
▲back to top |
 |
4.7 Page 37 |
▲back to top |
 |
4.8 Page 38 |
▲back to top |
 |
4.9 Page 39 |
▲back to top |
 |
4.10 Page 40 |
▲back to top |
 |
5 Pages 41-50 |
▲back to top |
 |
5.1 Page 41 |
▲back to top |
 |
5.2 Page 42 |
▲back to top |

 |
5.3 Page 43 |
▲back to top |
 |
5.4 Page 44 |
▲back to top |

 |
5.5 Page 45 |
▲back to top |

 |
5.6 Page 46 |
▲back to top |
 |
5.7 Page 47 |
▲back to top |






