Modern methods of
contraception
Male and female sterilization,
injectables, intrauterine devices
(IUCDs/PPIUCDs), contraceptive
pills, emergency contraceptive
pills, implants, female and male
condoms, diaphragm, foam/
jelly, standard days method
(a calendar-based method of
avoiding sexual intercourse on
fixed days to prevent pregnancy),
and lactational amenorrhoea
method (LAM – temporary
infertility after giving birth, when
a woman is not menstruating and
is fully breastfeeding).
Modern reversible
methods of contraception
Pill, intrauterine devices,
injectables, male condom,
female condom, emergency
contraception, lactational
amenorrhoea method (LAM).
Peer educators
Adolescents from the community
selected and trained to sensitise
and inform peers about their
health and well-being.
Unmet need
Proportion of women in the
reproductive age (15 to 49
years) who want to stop or delay
childbearing, but are not using
any method of contraception.
NFHS
The National Family Health
Survey (NFHS) is a large-scale,
multi-round survey conducted
since 1992-93 in a representative
sample of households, women
and men throughout India.
The survey provides district,
state and national information
on fertility, infant and child
mortality, family planning,
maternal and child health,
reproductive health, nutrition,
anaemia, utilisation and quality
of health and family planning
services.
What is the status, knowledge and access to SRH
services among adolescents and youth in India?
India’s large segment of young people will drive the country’s trajectory of
population growth for the next two to three decades8. Many of them have or will
soon join the reproductive age group (15 to 49 years). Fulfilment of their SRH needs
will have a significant and long-term impact, not only on population growth, but also
overall economic and development outcomes.
Recognising the needs of this group and the health risks it is exposed to in the
course of transition to adulthood, the Government of India adopted the Adolescent
Reproductive and Sexual Health Strategy in 2005, and the subsequent Rashtriya
Kishor Swasthya Karyakram (RKSK) or national adolescent health programme in 2014.
In addition, the National Population Policy (2000), the National Youth Policy (2014),
Rashtriya Yuva Sashaktikaran Karyakram (RYSK – 2016), the National Health Policy
(2017), the School Health & Wellness Programme (2020), and several other policy
commitments as well as programme initiatives address the needs of adolescents
and youth.
Menstrual health
One of the most significant physical
manifestations of puberty for girls is the
onset of menstruation. The government
has addressed menstrual hygiene
management for adolescent girls through
outreach under RKSK, awareness
generation, and distribution of sanitary
napkins at subsidised rates under the
Menstrual Hygiene Scheme, through
Pradhan Mantri Bhartiya Janaushadhi
Pariyojana (PMBJP) stores, and several
state government schemes.
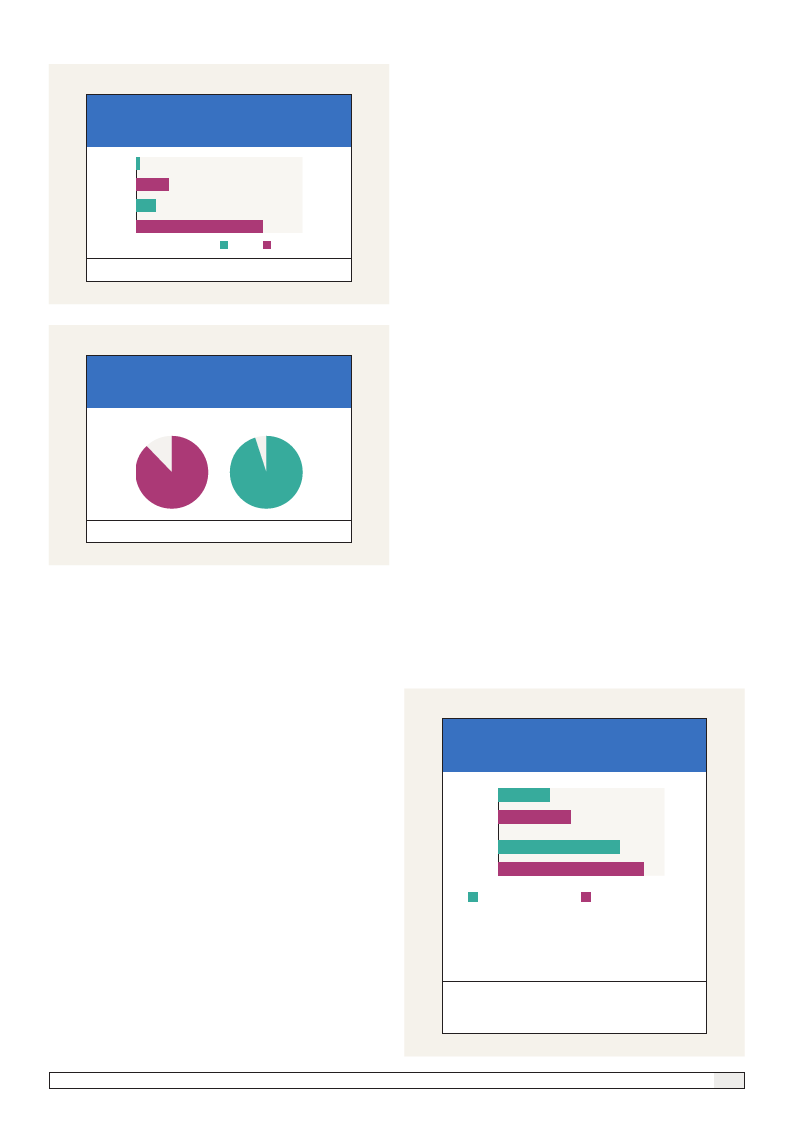
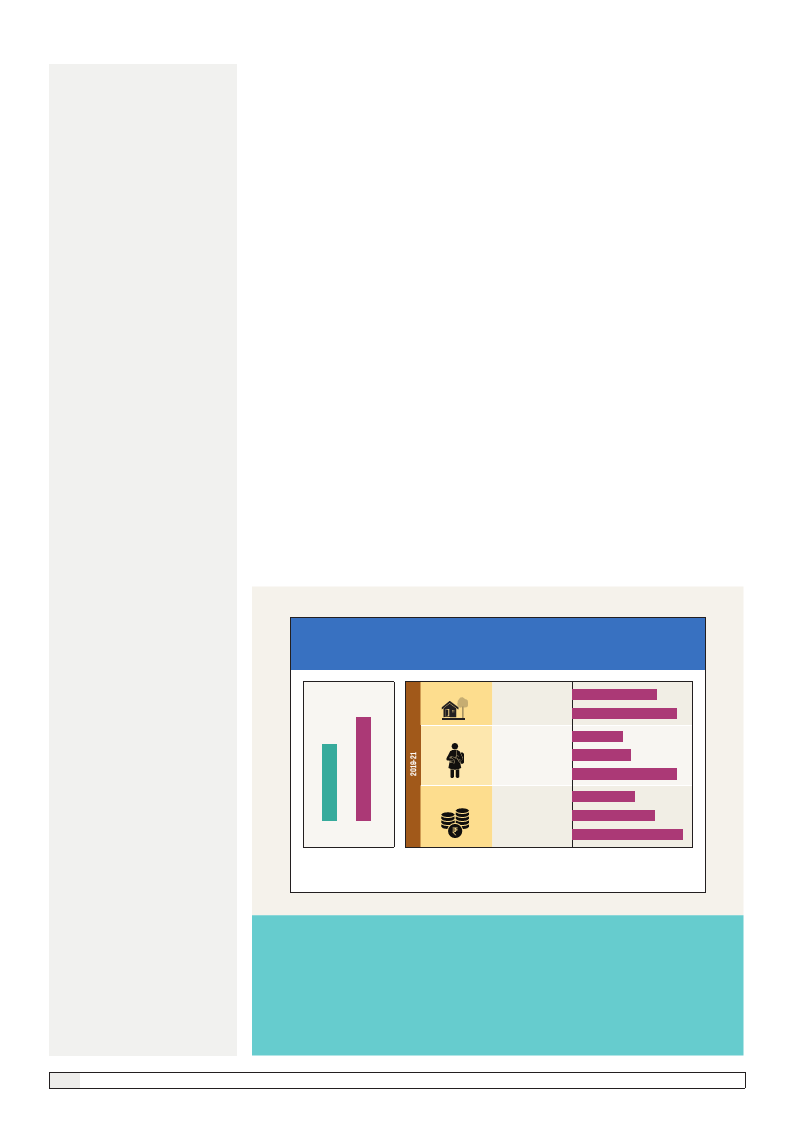
NFHS data shows that the use of
hygienic methods9 of menstrual health
management by 15 to 24 year-old women
increased by 20 percentage points
between 2015-16 and 2019-21 (Figure 1).
However, there are significant variations
in menstrual health management (MHM)
Figure 1
Percentage of women using hygienic method of protection*
during menstrual period, 2019-21
78
58
NFHS-4 NFHS-5
(2015-16) (2019-21)
Place of Residence
Rural
Urban
Schooling
No Schooling
< 5 years complete
≥ 12 years complete
Wealth Quintile
Lowest
Second
Highest
73
90
44
51
90
54
71
95
*Locally prepared napkins, sanitary napkins, tampons, and menstrual cups
For women in the age-group of 15 to 24 years who ever menstruated; Source: NFHS Rounds 4 & 5
Nine of 10 young women in urban areas use hygienic methods, as against
a little over seven of 10 in rural areas. Those with 12 or more years of
schooling are twice as likely to use hygienic methods compared to those
with no schooling. Young women in the lowest wealth quintile are 40
percentage points less likely to use hygienic methods compared to those
in the highest wealth quintile.
2
The sexual & reproductive health status of young people in India